Breakthrough Immunotherapy Revolutionizes Glioblastoma Treatment with Multi-Faceted Attack Strategy
2024-11-15
Author: Siti
Introduction
Glioblastoma (GBM), notorious for being the most prevalent and aggressive form of malignant brain tumor in adults, presents significant treatment challenges. The intricate tumor microenvironment (TME), coupled with the notorious blood-brain barrier, has stymied many therapeutic approaches. However, a pioneering immunotherapy developed by a team at the University of Basel and the University Hospital Basel shows promise in not only targeting glioblastoma cells but also reprogramming the TME to fight against the tumor.
The Research Team and Study Details
This groundbreaking research, recently published in *Nature Communications*, was spearheaded by Dr. Gregor Hutter, a leading professor at the University of Basel. The study is titled “Enhancing anti-EGFRvIII CAR T cell therapy against glioblastoma with a paracrine SIRPγ-derived CD47 blocker.”
Challenges in Current Treatments
Dr. Hutter and his colleagues confirmed that a major hurdle in effectively deploying chimeric antigen receptor (CAR) T cell therapy against GBM is the tumor’s immunosuppressive microenvironment, teeming with tumor-promoting glioma-associated microglia and macrophages (GAMs). Traditional approaches focusing solely on targeting CD47 to unleash these immune cells have faced significant challenges; toxicity and poor effectiveness in solid tumors have made these treatments less viable.
Innovative Approach
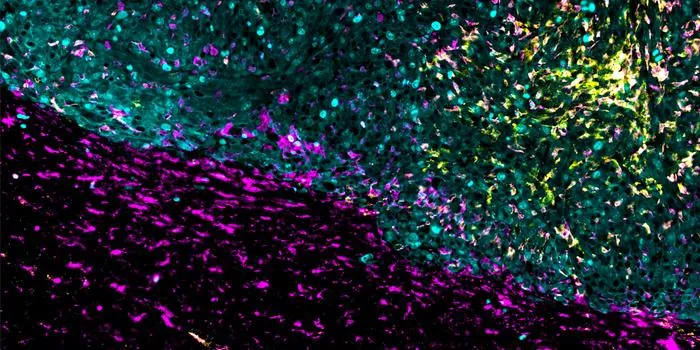
The innovative approach taken by Hutter's team involved engineering CAR T cells specifically targeting the epidermal growth factor receptor variant III (EGFRvIII). These specially designed T cells secrete proteins that effectively block CD47's signaling, allowing immune cells to operate more effectively. This dual attack not only directs T cells towards the glioblastoma cells but also invigorates the surrounding microglia and macrophages to join the fight against the tumor.
Direct Administration of CAR T Cells
Moreover, the researchers are exploring the possibility of administering the modified CAR T cells directly into the tumor, thus bypassing the daunting challenge of getting these cells to penetrate brain tissue. The altered T cells are given a genetic instruction to produce a signaling molecule that mitigates the tumor’s attempts to suppress immune response, transforming GAMs into allies rather than foes.
Initial Trials and Results
Initial trials in mice, implanted with human glioblastoma cells, yielded promising results, showing a complete eradication of cancer cells. Encouragingly, this method has also shown effectiveness against lymphoma in preliminary testing.
Next Steps and Future Considerations
As the next step, the research team aims to transition this innovative therapy into a clinical study involving patients. Dr. Hutter expressed optimism, noting that localized injections would likely minimize systemic side effects compared to traditional systemic therapies. Nonetheless, the team remains cautious about potential adverse effects on the nervous system, which have been observed in prior CAR T cell therapies.
Conclusion
This breakthrough could not only change the landscape of glioblastoma treatment but also pave the way for more effective strategies against other forms of solid tumors. Scientists and clinicians alike are eager to see how this transformative immunotherapy can offer hope to patients battling one of the most formidable cancers known to medicine. Stay tuned for updates on upcoming clinical trials!


 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)