Breakthrough CAR T Cell Therapy Aims to Overcome Glioblastoma Challenges While Protecting Healthy Brain Tissue
2024-09-27
In a groundbreaking development, researchers from the University of Geneva (UNIGE) and the Geneva University Hospitals (HUG) have engineered CAR T cells specifically designed to target glioblastoma, the deadliest and most common primary brain tumor, all while sparing healthy tissue. With an alarmingly short average survival rate of less than two years post-diagnosis, glioblastoma has long posed a significant challenge to traditional therapies. However, recent advancements in immunotherapy are igniting new hope for patients battling this aggressive cancer.
The frustration with conventional treatments, including surgery, chemotherapy, and radiation, is that they often fail to provide lasting results. Glioblastomas are not only notorious for their rapid recurrence but also for creating an immune-suppressive microenvironment that thwarts the body’s defense systems. This breakthrough research highlights a specific marker, PTPRZ1, found on the surface of tumor cells, which plays a pivotal role in enhancing the efficacy of CAR T cell therapy.
Denis Migliorini
An expert in brain tumor immunology and an assistant professor at UNIGE, concentrated efforts on pinpointing the protein markers unique to glioblastoma cells. "Through rigorous study, we identified PTPRZ1 as a vital target. We successfully produced CAR T cells that can recognize and attack cells carrying this marker," he explained. This significant step shows promise for the potential treatment of malignant gliomas, a cancer that has sorely needed effective therapies.
Customization for Enhanced Efficacy
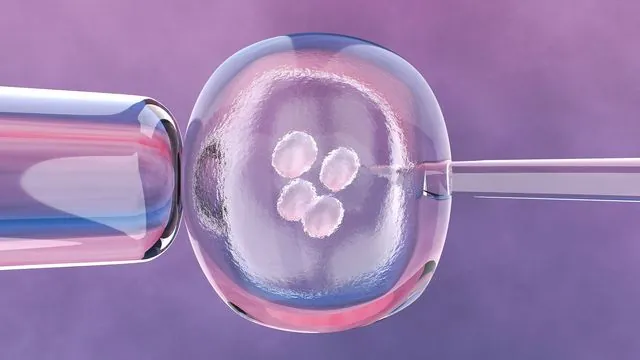
In an innovative twist, instead of relying on viral vectors, which can be problematic in sensitive brain environments, the team incorporated messenger RNA into T cells. This method instructs cells to generate antibodies capable of targeting glioblastoma, offering a more adaptable platform capable of responding to tumor evolution. "This adaptability enhances the treatment’s potential effectiveness against the ever-changing landscape of cancer," notes Darel Martinez Bedoya, a post-doctoral researcher involved in the project.
A Game-Changing Response: Efficacy and Safety Simultaneously
Initial testing revealed that these specially engineered CAR T cells not only avoided attacking healthy cells but demonstrated an extraordinary ability to eliminate tumor cells that did not express the PTPRZ1 marker. Disturbingly, glioblastoma cells can often evade direct targeting, making this "bystander effect" significant.
The research team then proceeded to test CAR T therapy in mouse models that mimic human glioblastoma. The results were overwhelmingly positive, showcasing a remarkable control over tumor growth and notable life extension without evident toxicity. "By delivering CAR T cells directly into the tumor in the central nervous system, we substantially reduce the risk of adverse effects on surrounding healthy tissue," Migliorini added.
A Future Full of Promise
With the compelling results from these preliminary studies, the research team is poised to move forward with plans for clinical trials involving human patients. As glioblastoma remains one of the fiercest adversaries in oncological research, advancements like this CAR T cell therapy offer not only a glimmer of hope but could potentially revolutionize the treatment landscape for this and other hard-to-treat cancers.
This remarkable advancement highlights not only the scientific prowess at UNIGE and HUG but also the relentless pursuit of solutions in the face of daunting challenges. As the clinical trials approach, the medical community watches with bated breath, eager for a new chapter in the fight against glioblastoma.


 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)