Antithrombotic Therapy's Impact on Gastrointestinal Bleeding: Study Insights Revealed
2025-09-10
Author: Li
Understanding Gastrointestinal Bleeding in Antithrombotic Patients
Gastrointestinal (GI) bleeding is a pressing concern often leading to emergency room visits. It can arise from various sources—both upper and lower GI—but pinpointing the exact location can be challenging upon patient admission. This study delves into how antithrombotic therapy, involving medications like anticoagulants and antiplatelet drugs, can influence bleeding symptoms, identification of bleeding sources, and subsequent treatment strategies.
Study Overview and Methodology
Conducted at Skåne University Hospital, this research analyzed data from 585 adult patients admitted for GI bleeding between January 2018 and June 2019. Patients were divided based on their antithrombotic status (either on therapy or not), allowing for a thorough comparison of bleeding presentations and treatment outcomes.
Key Findings: Who is Affected?
Among the patients studied, 54% were on some form of antithrombotic medication. Notably, patients on these therapies tended to be older and had higher comorbidity scores, suggesting they might present unique challenges in emergency care. Despite these differences, preliminary bleeding indicators like hemoglobin levels and shock index showed no significant variation across the groups.
Shocking Differences in Bleeding Symptoms
The study unveiled striking differences in the symptoms exhibited by patients on antithrombotics. For instance, those receiving anticoagulant therapy were less likely to present with hematemesis (vomiting blood), significantly contrasted by patients not on antithrombotic treatment. Instead, a greater proportion of patients on anticoagulants presented with hematochezia (bloody stools), implying that antithrombotic medication could skew the presentation of GI bleeding.
Identifying the Bleeding Source
Despite variations in initial symptoms, the study found no significant disparity in the successful identification of the bleeding source among the groups. However, patients on anticoagulant therapy had a notably lower chance of having a bleeding source pinpointed compared to those on antiplatelet therapy or those not taking any antithrombotics.
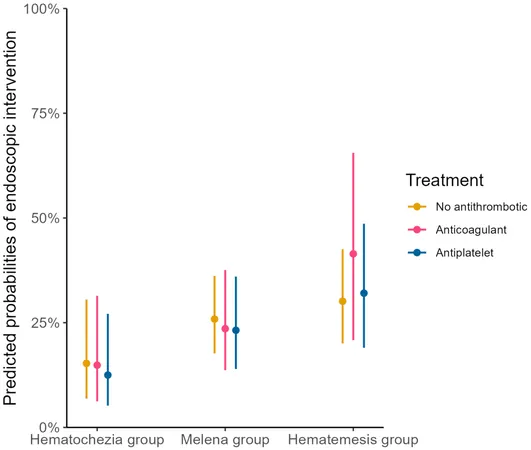
Treatment and Outcomes: No Difference?
Interestingly, the need for endoscopic treatments, blood transfusions, or surgical interventions did not differ significantly between the groups. This suggests that while initial presentations may vary, the overall treatment required for GI bleeding may be similar across patients, regardless of their antithrombotic medication status.
Conclusion: What Does It All Mean?
The study highlights the pivotal role antithrombotic medications play in altering the presentation of gastrointestinal bleeding. While patients with these therapies often exhibit different bleeding symptoms, it appears that the actual need for urgent interventions remains consistent across all groups. As emergency practitioners face an increasingly aged patient demographic, understanding these nuances could enhance diagnostic assessments and treatment protocols in the face of GI bleeding.
 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)