Antibiotics May Harm Gut Health: New Insights into IBD and Mucus Layer Disruption
2025-03-24
Author: Wei
Recent Research on Antibiotics and Gut Health
Recent research has unveiled a concerning truth about antibiotic use and its unintended consequences on gut health, particularly linking it to inflammatory bowel disease (IBD). While antibiotics are prescribed mainly to eradicate harmful bacteria, the potential harm to the body’s beneficial bacteria and structures, such as the protective mucus barrier in the intestines, is often overlooked.
The Hidden Effects of Antibiotics
Shai Bel, an immunologist at Bar-Ilan University, aimed to uncover the mechanisms behind how antibiotics might contribute to the onset of IBD. He stated, “We have treatments to subdue the immune response, but we aren't addressing the root cause because we do not fully understand what it is.”
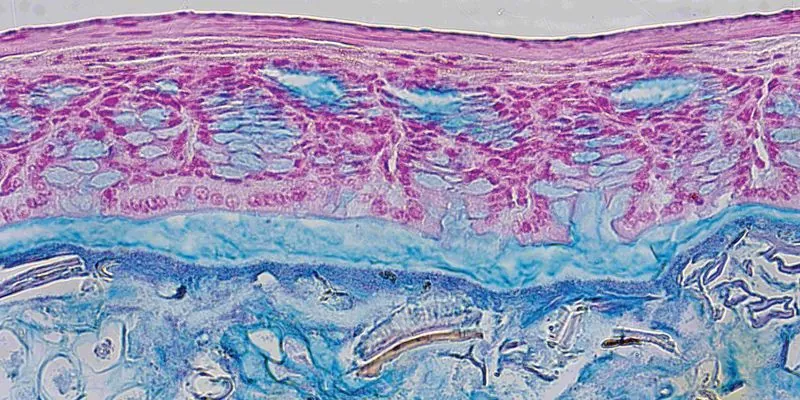
In groundbreaking experiments with mice, Bel's research team observed that a variety of antibiotics, spanning four different classes, inflicted significant damage to the gut's mucus layer. This mucus layer is crucial as it acts as a barrier separating intestinal epithelial cells from the microbes residing in the gut lumen. Bel noted, “From our initial experiments, it was abundantly clear that antibiotic treatment resulted in the complete disappearance of the mucus layer.” Without this protective barrier, bacteria can cling to the epithelial cells, triggering immune responses that can escalate into harmful inflammation.
Immune System Overdrive: A Recipe for IBD
Bel hypothesizes that in humans, the absence of the mucus barrier could lead the immune system to go into overdrive, perpetually reacting to the bacteria it senses, a potential precursor to developing IBD.
To explore the causes of this mucus layer deterioration, his team administered vancomycin and neomycin systemically to the mice. The results were alarming; these antibiotics activated genes associated with endoplasmic reticulum (ER) stress, resulting in decreased mucus production by the gut epithelial cells. However, there was a silver lining: by administering a molecule that mitigates ER stress, they were able to restore mucus secretion from these cells.
Looking Ahead: Possible Solutions for Humans?
Current studies are focused on whether boosting mucus secretion can alleviate inflammation in IBD models. Bel expressed hopes for future human studies, asserting that the proposed treatment could help restore gut health without compromising the immune system, in contrast to existing therapies. He stated, “Our approach is to allow the immune system a chance to recover, rebuild the barrier, and ideally, the immune system can heal itself.”
This pivotal research stresses the need for healthcare providers to prescribe antibiotics with greater caution. As Bel pointed out, “There’s this unwritten rule that antibiotics should only target harmful microbes and not harm us. This notion has led to their widespread use, often without careful consideration.” He cautioned, “We can’t continue prescribing them so liberally.”
As we further explore the complexities of gut health, this research serves as a critical reminder that our medical practices must evolve in tandem with new scientific understanding. Will this lead to a re-evaluation of antibiotic prescriptions in the future? Only time will tell, but the stakes for gut health and overall wellbeing are undeniably high.




 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)