Alarmingly Low Predictive Power of Biomarkers for Pulmonary Oedema in Severe Malaria Patients Revealed in New Study
2024-10-24
Author: Siti
Overview
Pulmonary oedema, a serious and often unpredictable complication of severe falciparum malaria, can arise shortly after the initiation of antimalarial treatment, posing a significant challenge for healthcare providers. This condition is primarily influenced by proinflammatory mediators, which are believed to exacerbate pulmonary complications. A new prospective observational study conducted in Bangladesh aimed to evaluate the effectiveness of various biomarkers in predicting the onset of clinical pulmonary oedema in patients with severe falciparum malaria.
Study Design and Methodology
The study included 106 individuals diagnosed with falciparum malaria, with 56 patients classified as experiencing severe malaria, highlighting a concerning 29% mortality rate in this group. The research focused on biomarkers such as interleukin-6 (IL-6), interleukin-8 (IL-8), tumor necrosis factor (TNF), and others, assessing their plasma concentrations upon hospital admission. Comparisons were made to a control group of healthy individuals to explore any potential correlation with pulmonary oedema development.
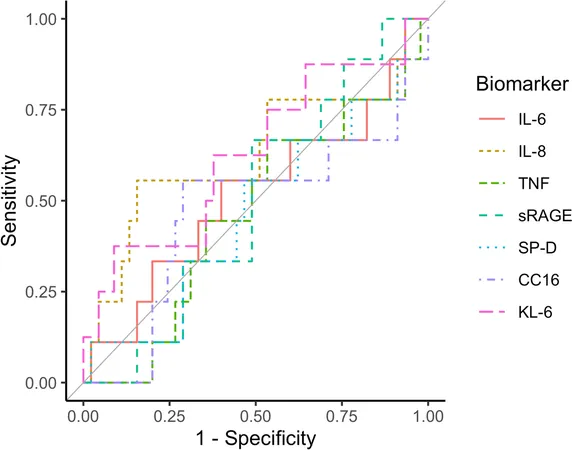
Despite elevated levels of biomarkers in patients compared to controls, the results indicated that none of these markers could reliably predict the occurrence of clinical pulmonary oedema. Specifically, while there were strong correlations between certain biomarkers and known prognostic factors like plasma lactate and Plasmodium falciparum histidine-rich protein 2 (PfHRP2), the predictive power for pulmonary complications remained significantly low.
Findings and Implications
Out of the severe malaria cohort, 16% (nine patients) developed clinical pulmonary oedema after being admitted to the hospital. Nevertheless, the expected predictive capacity of various biomarkers was not demonstrated; even proinflammatory mediators did not correlate with the onset of oedema. The lack of predictive value of these biomarkers raises critical questions about their role in managing severe malaria complications.
As malaria continues to be a pressing public health issue, especially in the aftermath of the COVID-19 pandemic, this study underscores the urgency for improved diagnostic tools and management strategies. With pulmonary oedema being associated with high mortality rates, the inability to forecast its onset can complicate treatment efforts, particularly in resource-limited settings where advanced respiratory support may be unavailable.
Further Insights
The pathophysiology of pulmonary oedema in severe malaria is complex and poorly understood. Proinflammatory cytokines are thought to damage lung endothelial cells, increasing pulmonary capillary permeability, but the timing of its onset complicates the connection to traditional prognostic mechanisms. This signals a potential need for ongoing research into the exact mechanisms behind pulmonary involvement in severe malaria cases.
Future investigational studies could expand on these findings by utilizing longitudinal analyses to capture the dynamics of biomarker levels post-hospital admission. Such insights might lead to the identification of novel predictive biomarkers, enhancing the clinical management of severe malaria and preventing catastrophic outcomes.
In summary, the alarmingly low predictive capacity of traditional biomarkers for pulmonary oedema in severe malaria patients poses a significant concern, emphasizing the need for innovative approaches in both research and clinical practice. As the world grapples with the complexities of malaria management, prioritizing the optimization of diagnostic tools will be essential in saving lives.

 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)