Alarming Trend: Medicare Enrollment Linked to Decreased Mental Health Care Access for Seniors
2025-01-17
Author: Rajesh
Introduction
A recent study from the USC Schaeffer Center for Health Policy & Economics has unveiled a troubling reality: as individuals transition into Medicare at age 65, those from low- and middle-income backgrounds experience a dramatic decrease in access to mental health care services.
Study Findings
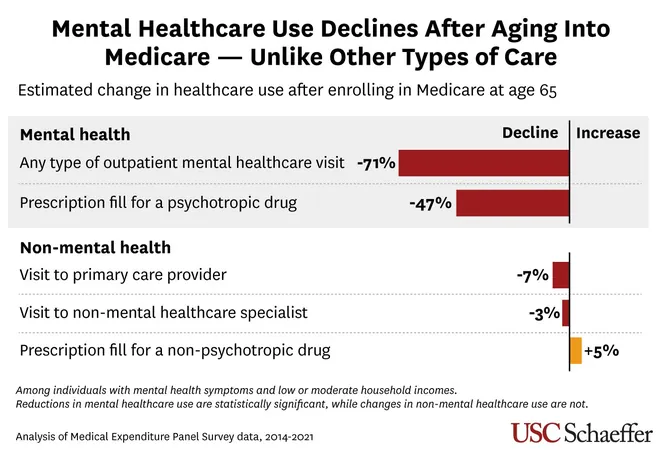
The research revealed a shocking 71% drop in the likelihood of utilizing outpatient mental health services among these individuals after enrolling in Medicare. Furthermore, their chances of being prescribed psychotropic medications, including antidepressants and mood stabilizers, fell by 47%. Disturbingly, these trends held true for both traditional Medicare and Medicare Advantage plans.
Concerns Raised
Concerns about access to mental health care for Medicare beneficiaries have been mounting due to the program's coverage limitations and a notable shortage of participating mental health providers. The study published in Health Services Research is pioneering in its examination of how aging into Medicare affects mental health service utilization among those showing probable symptoms of mental health issues.
Expert Insights
Lead researcher Grace McCormack emphasized the seriousness of these findings: “People with substantial mental health needs seem to receive drastically less mental health care once they age into Medicare. This is particularly worrisome, given the escalating demand for mental health services among the over-65 demographic.
Contrasting Trends
Remarkably, the data also indicated that Medicare enrollment did not influence the frequency with which individuals sought care from non-mental health providers or filled prescriptions for non-psychotropic drugs. This suggests that while Medicare provides coverage, it may unintentionally create specific barriers to accessing necessary mental health care for vulnerable populations who cannot afford out-of-pocket expenses.
Income Disparities
In a contrasting trend, individuals with mental health symptoms from higher-income households did not report any decline in mental health visits; rather, their use of psychotropic medication increased after enrolling in Medicare. This disparity highlights the complexities of mental health care access, which can vary significantly based on economic background.
Methodology
The study utilized a robust nationally representative survey, shedding light on patterns of healthcare use, spending, and insurance coverage from 2014 to 2021. With the rising recognition of mental health as a critical aspect of overall well-being, these findings urge a reevaluation of Medicare policies to ensure that all seniors, regardless of income level, have appropriate and effective access to mental health services.
Conclusion
As we continue to address the growing mental health crisis, particularly among older adults, it raises a pressing question: How can we reform Medicare to better support the mental health needs of our aging population? It's time for policymakers to take action before the situation worsens.


 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)