Alarming Rise in Antimicrobial Resistance: What You Need to Know!
2025-03-20
Author: Wei
In a groundbreaking 10-year study, the Centers for Disease Control and Prevention (CDC) revealed a troubling trend: while antimicrobial resistance in hospitals saw a decline from 2012 to 2019, the COVID-19 pandemic years (2020-2021) marked a significant reversal, with a notable increase in resistant infections. Researchers are calling attention to the urgent need for enhanced infection prevention strategies across healthcare settings.
Overview of the Study
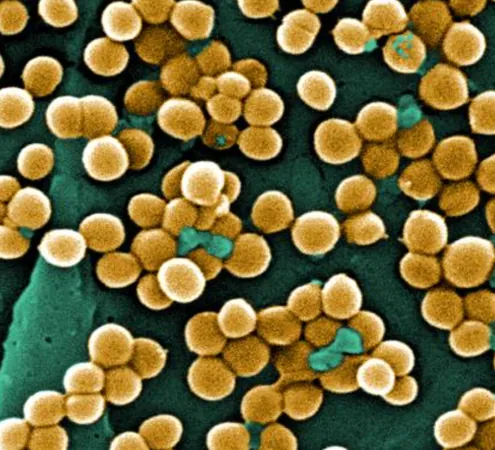
The study analyzed six major pathogens that pose a significant threat to public health: methicillin-resistant Staphylococcus aureus (MRSA), vancomycin-resistant Enterococcus spp (VRE), extended-spectrum cephalosporin-resistant Escherichia coli and Klebsiella spp (collectively referred to as ESCR-EK), carbapenem-resistant Enterobacterales (CRE), carbapenem-resistant Acinetobacter spp (CRAsp), and multidrug-resistant (MDR) Pseudomonas aeruginosa. The CDC, alongside the World Health Organization, has classified these pathogens as high-priority targets for intervention.
Findings of Resistance Rates
According to the findings published in JAMA Network Open, the rates of resistance for MRSA, VRE, CRE, CRAsp, and MDR Pseudomonas aeruginosa remained stable or showed declines from 2012 to 2022. However, the percentage of ESCR-EK infections, particularly among nonsterile and sterile body sites, surged—rising from 12.2% to 19.7% and from 17.5% to 24.5%, respectively. This spike indicates a worrisome trend that healthcare professionals must address immediately.
Regional Differences in Resistance Rates
The reductions in CRE rates were not uniform; while the Northeast U.S. saw a decrease in hospital-onset CRE infections, rates in other regions either stabilized or continued to rise. Additionally, significant demographic disparities were noted: male patients and older age groups (particularly those aged 55-74) experienced higher rates of these hospital-onset resistant infections.
Pandemic Impact on Antimicrobial Resistance
This comprehensive cohort study, which spanned data from 2012 to 2022, included detailed analyses of inpatient hospitalizations, clinical cultures, and various facility characteristics. Cases of interest were identified using robust methodologies, ensuring a high standard of research rigor.
But why did the pandemic exacerbate these issues? The investigators pointed to several factors during the acute phase of COVID-19 that could have influenced resistance patterns—decreased overall hospital admissions, an influx of high-risk COVID-19 patients, and the presence of sicker non-COVID-19 patients seemingly contributed to this alarming increase. Moreover, the average length of hospital stays rose significantly from 2020 to 2022, which correlates strongly with the likelihood of developing hospital-acquired infections.
They also highlighted a decline in infection control practices during the pandemic, noting that reductions in contact precautions and oversight of antimicrobial use may have permitted increased resistance to take root.
Need for Strategic Action
Unquestionably, strategic action is essential. The CDC emphasizes that preventive measures must be prioritized, especially in contexts of heightened healthcare demand, like during the pandemic. Failing to adapt infection prevention efforts could lead to further increases in resistant infections, putting additional strain on hospitals and patients alike.
Conclusion
The data suggest that a rigorous, consistent approach to infection control is paramount in navigating this ongoing crisis. As we emerge from the pandemic, addressing these resistance trends with innovative solutions becomes critical to safeguarding public health and preserving the efficacy of antibiotics for future generations.
Call to Action
Are you aware of the growing threat of antimicrobial resistance? What measures do you think hospitals should adopt to combat this issue?


 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)