Alarming Prevalence of Common Mental Disorders in Non-Psychiatric Wards: A Study from Eastern Ethiopia Highlights the Hidden Crisis
2025-01-17
Author: Ming
Introduction
In a significant public health revelation, a recent study has unveiled the troubling prevalence of common mental disorders (CMDs) among adult patients admitted to non-psychiatric wards in public hospitals of Harari regional State, Eastern Ethiopia. Common mental disorders are often overlooked yet critical issues that complicate medical care and seriously affect patient outcomes. They lead to increased treatment costs, longer hospital stays, and a higher risk of complications and mortality.
The Research Study
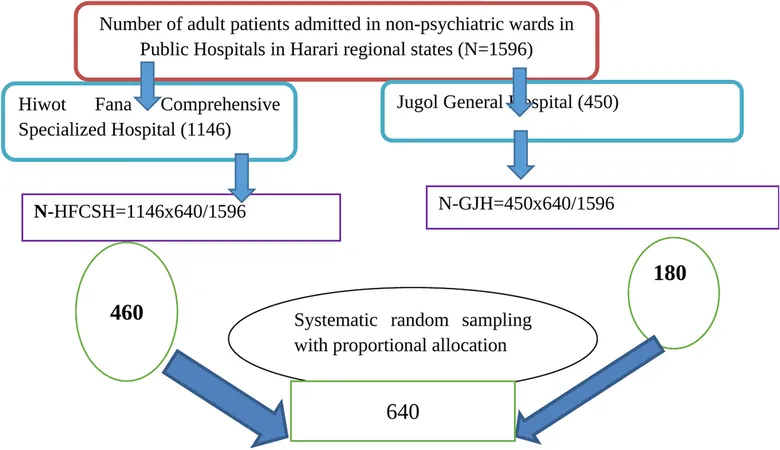
Conducted between November 15 and December 15, 2022, the study surveyed 640 patients admitted to non-psychiatric wards, employing a systematic random sampling technique. Data collection utilized structured questionnaires, including the Self-Report Questionnaire-20 (SRQ-20) to identify the presence of CMDs. Analysis was performed using sophisticated statistical methods, highlighting various factors significantly associated with these disorders.
Key Findings
The startling results revealed that 45.3% of adult patients exhibited symptoms of CMDs, a statistic grounding itself within a 95% confidence interval of 41.3% to 49.2%. Key factors linked with CMDs included: - Age: Patients aged 41-51 (AOR = 1.732) and those over 51 (AOR = 2.429) exhibited higher odds of experiencing CMDs. - Length of Hospital Stay: Those hospitalized for 1-2 weeks (AOR = 1.743) and over four weeks (AOR = 2.12) were significantly affected. - History of Mental Illness: A staggering AOR of 5.841 highlighted that those with previous mental health conditions are more susceptible to CMDs. - Stressful Life Events: Experiencing life stressors increased the likelihood of CMDs (AOR = 1.876). - Substance Use: Patients currently using substances showed 1.688 times the odds of developing CMDs compared to non-users. Moreover, poor social support dramatically increased CMD odds (AOR = 2.562), underscoring the role of community support in mental health.
Contextual Background
Globally, over 450 million people suffer from CMDs, with community prevalence rates ranging from 14% to 15%. Yet, hospitals frequently witness higher rates due to undiagnosed cases, where CMDs masquerade as physical ailments. These mental disorders generate significant health burdens, with many individuals in developing countries like Ethiopia left untreated.
A Call to Action
The study's authors advocate for the integration of mental health screenings into routine care for all patients admitted to non-psychiatric wards. With such high prevalence rates and the association of CMDs with increased morbidity and treatment costs, the need for comprehensive mental health support systems has never been more urgent.
Final Thoughts
As healthcare professionals and policymakers strive to identify and address mental health concerns, the findings from this study call for urgent reforms in how mental health is perceived and managed within clinical settings, particularly in resource-limited countries. This hidden crisis of common mental disorders in non-psychiatric wards cannot be ignored any longer; proactive measures are essential not only for improving patient care but for enhancing overall healthcare outcomes in Ethiopia and beyond. Stay tuned for groundbreaking insights on mental health initiatives and strategies aimed at combating this pressing public health issue!


 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)