Alarm Bells Ring: Hong Kong Faces Continued Depression Crisis and Rising Healthcare Costs Until 2032!
2024-11-15
Author: Ming
Alarm Bells Ring: Hong Kong Faces Continued Depression Crisis and Rising Healthcare Costs Until 2032!
In a groundbreaking study led by Professor Shirley Li Xue from the University of Hong Kong's LKS Faculty of Medicine, experts have projected that Hong Kong will grapple with a significant and relentless burden of depression from 2023 to 2032. This first-of-its-kind health economic modeling research, published in The Lancet Regional Health – Western Pacific, reveals alarming statistics that shed light on the shifting landscape of mental health in the region.
Despite fewer than 20% of depression patients anticipated to develop treatment-resistant depression (TRD) or additional mental health complications, this small yet critical group is expected to account for nearly half of the city's depression-related healthcare costs. With the backdrop of global socioeconomic shifts post-COVID, the study emphasizes the urgent need for multidisciplinary health and social support systems in Hong Kong.
As mental health concerns have surged in the wake of the pandemic, Hong Kong is no outlier. The research team has crafted a comprehensive health economic model aimed at forecasting both the costs of care and mortality associated with depression over the next decade. This proactive approach aims to facilitate long-term resource planning and ensure that health systems are primed to meet the growing demand for mental health services.
Utilizing extensive electronic medical records from the Hospital Authority, the study analyzed a cohort of over 25,000 depression patients diagnosed between 2014 and 2016, tracking their outcomes up until 2020. This large-scale real-world data initiative informed a Markov-chain-based model, which meticulously delineates patient experiences from initial diagnosis through potential treatment resistance and comorbidities.
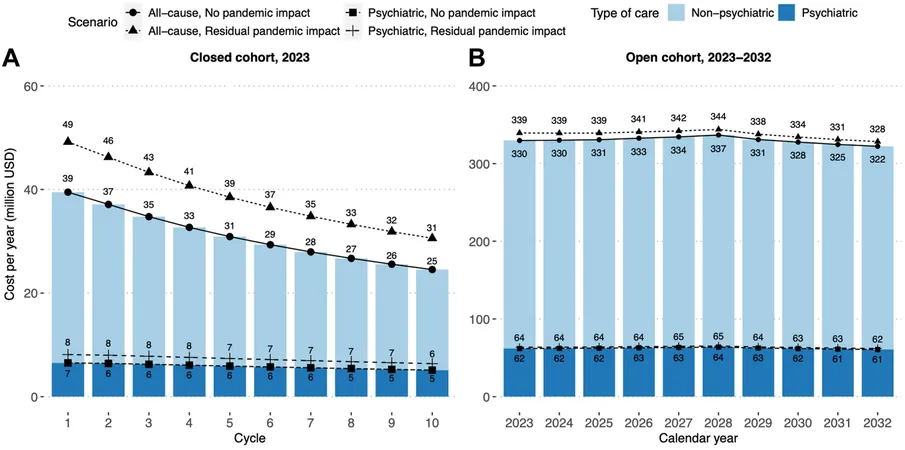
The forecast under a "status quo" scenario—where no new treatment strategies are implemented—paints a grim picture: an estimated 55,849 to 57,896 individuals will experience depression annually through 2032, incurring healthcare costs exceeding HK$2.51 billion, with psychiatric care alone costing HK$473.5 million. Alarmingly, these costs are predicted to stabilize over the next ten years without any new interventions considered.
Vulnerable groups, undeniably, will bear the brunt of this burden. Although men are statistically less likely to suffer from depression, once diagnosed, they tend to consume more healthcare resources. Elderly men with prior health conditions face the highest individual costs and mortality risks, while costs for adolescent patients requiring psychiatric care could be the most substantial.
Early intervention emerges as a critical factor for mitigating these costs. Less than 20% of those battling depression are predicted to encounter TRD; however, this group will account for a staggering 31% to 54% of total depression-related healthcare expenditures. Timely intervention is crucial as the more severe stages of depression present the most significant challenges and expense.
"This study offers essential insights for the strategic planning of mental health resources in Hong Kong," stated Professor Li. "Policymakers must recognize the ongoing challenge posed by depression and prioritize budget allocations for at-risk populations, such as adolescents and individuals with pre-existing medical issues."
To combat this looming crisis, experts underscore the necessity of establishing early intervention programs aimed at patients most likely to transition to TRD. The research team's innovative modeling can simulate various treatment scenarios and provide predictions on how changes in therapy could alter the cost burden on the healthcare system.
As the study continues to investigate multiple therapeutic avenues, it highlights the necessity for adaptability within Hong Kong's health services to effectively respond to the anticipated long-term mental health care needs of its population. The wake-up call for immediate, structured solutions has never been more urgent as the city steels itself for the challenges ahead.

 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)