AI's Role in Colonoscopy: Victory in Polyp Detection, but Limited Impact on Cancer Risk
2025-03-28
Author: Sarah
Introduction
A groundbreaking study from a team of Norwegian researchers, in collaboration with international experts, reveals that the integration of artificial intelligence (AI) during colonoscopy screenings has significantly enhanced the detection of polyps by approximately 8%. However, this increase comes with a crucial caveat: the effect on the actual risk of developing colorectal cancer remains minimal.
The Importance of Colorectal Cancer Screening
Colorectal cancer is a pressing concern, especially in the Western world, where it ranks as one of the most prevalent cancers. In Norway alone, around 5,000 individuals are diagnosed with colorectal cancer annually. To combat this growing issue, Norway has recently launched a national screening initiative aimed at early detection of this disease.
Current Screening Practices
Traditionally, colorectal cancer screening in Norway has utilized fecal immunochemical tests (FIT), which detect blood in stool samples. If the screening indicates the presence of blood, patients are then referred for a more comprehensive colonoscopy. In a significant shift, the Norwegian Directorate of Health has announced plans to replace the stool test with colonoscopies for every citizen turning 55 within the next five years.
The Role of AI in Colonoscopy
During these colonoscopic evaluations, AI is frequently employed as a supportive tool to identify polyps that may indicate cancerous developments. This technological advancement comes as part of a broader initiative to ensure that the benefits of AI in healthcare are thoroughly documented. To this end, international guidelines for AI application in colonoscopy have been developed, spearheaded by the Norwegian-based MAGIC foundation and published by BMJ Rapid Recommendations.
Research Findings
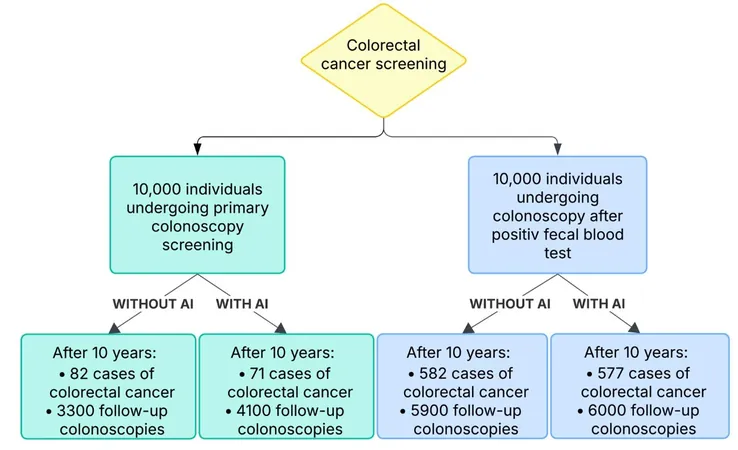
A recent extensive microsimulation study, conducted by researchers at the University of Oslo, sought to analyze the implications of AI on cancer prevalence and mortality rates, taking into account the increased burden of follow-up colonoscopies due to heightened polyp detection. This comprehensive analysis reviewed data from around 15 relevant studies, adding depth to the existing body of research.
Guidelines and Recommendations
The findings were disseminated urgently in BMJ Medicine to inform the updated guidelines. Researcher Natalie Halvorsen noted, “While AI can indeed improve the detection of polyps, its impact on cancer risk is quite modest. The balance between enhancing detection and the potential for increased follow-up examinations still needs thorough evaluation.”
The newly released guidelines articulate a cautious approach, advising against the routine implementation of AI for general colonoscopy screening in adults. There is a recognition of the uncertainty surrounding these recommendations, prompting calls for further health economic assessments to refine future updates.
Divergent Views in Guidelines
In a parallel development, the American Gastroenterology Association (AGA) and the European Society of Gastrointestinal Endoscopy (ESGE) have issued their own guidelines regarding AI's application in colonoscopy this week. Contradicting BMJ’s stance, the AGA has opted not to endorse AI usage either for or against, while the ESGE supports AI implementation, suggesting a majority of patients would prefer such assistance.
Conclusion
Halvorsen added, “The variance in recommendations underscores the complexity of integrating AI in healthcare, balancing its inherent benefits against the risks of overdiagnosis and an overwhelmed health system.” Professor Per Olav Vandvik, founder of MAGIC and leader of the BMJ Rapid Recommendations project, emphasized the importance of ongoing collaboration and adaptation in the rapidly evolving field of AI medicine. “We've shown that while we have robust methods to evaluate AI, we need to be prepared to update those methods dynamically, just as we did for COVID-19,” he stated.
The findings also revealed critical insights regarding the burden placed on patients and healthcare systems associated with the adoption of AI. Specifically, the study indicated a minimal clinical effect from AI on cancer risk, with a 10-year reduction rate from 0.82% without AI to 0.71% with AI. Conversely, the use of AI led to a 20% increase in follow-up colonoscopies, further straining healthcare resources.
In summary, while AI has the potential to enhance polyp detection during colonoscopies, its effect on reducing cancer risk remains limited, emphasizing the need for careful consideration of both its benefits and drawbacks before widespread adoption in clinical practice.
 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)