Adapting Digital Competencies in Canada's Public Health Workforce: Insights from Practitioners
2025-01-10
Author: Nur
The rapid digital revolution sweeping through public health and society at large has underscored an urgent need for new digital competencies among public health professionals. The COVID-19 pandemic further accelerated this transformation, necessitating the incorporation of numerous digital tools aimed at improving public health responses. Recognizing this, Canadian public health organizations have set out to equip their workforce with the necessary skills to adapt and leverage these tools for enhanced disease surveillance, informed decision-making, and more effective outreach to underserved populations.
According to recent studies, the era of misinformation—exacerbated by social media—calls for public health practitioners to not only master digital technology but also to adeptly address challenges stemming from disinformation. For example, global studies have illustrated a troubling correlation between misleading online information and declining vaccination rates, highlighting a pressing need for digital literacy in today's health landscape.
To address this pressing issue, researchers conducted a comprehensive three-phase study focused on identifying key digital competency needs for Canadian public health training programs. The initial phase involved a rapid review, revealing a general consensus about the necessity of digital skills, though specific guidelines and recommendations were sparse. The findings highlighted that the recommended competencies spanned all categories laid out by the Public Health Agency of Canada (PHAC), including newly identified skills for managing digital data streams.
Canada’s unique public health landscape—marked by a decentralized and universal health system—presents particular challenges in establishing a cohesive approach to digital competency development. With a complex web of health authorities across ten provinces and three territories, varying resource allocation, and specific jurisdictional mandates, developing a unified framework is crucial. Moreover, Canada's commitment to addressing Indigenous health disparities mandates an equitable approach in equipping all segments of the population, including practitioners from diverse backgrounds.
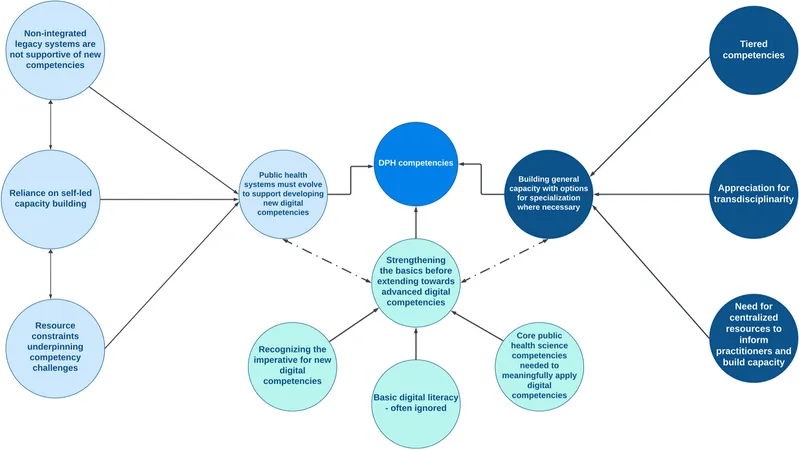
The third phase of the study focused on contextualizing internationally recognized competency and training recommendations. By engaging public health professionals across different regions in focus group discussions, the study uncovered three pivotal themes necessary for effective digital competency training:
1. Evolution of Public Health Systems
Participants emphasized that existing digital infrastructures often complicate—not facilitate—public health operations. Many health workers cited experiences with fragmented systems and outdated technologies, leading to inefficient data management. Addressing these structural issues is essential for fostering the digital competencies that public health workers need.
2. Foundation First
Participants voiced the critical need to first solidify basic digital skills before moving towards more specialized competencies. A robust understanding of fundamental areas—such as biostatistics, public health sciences, and digital data communication—serves as an essential groundwork for practitioners. Without these core skills, advanced technological training would yield limited benefits.
3. General and Specialized Competencies
The study revealed the necessity for a balanced approach—public health professionals should possess both a broad understanding of digital technologies and opportunities for specialization. This means creating pathways for advanced digital skills in areas like data science and public health informatics, while simultaneously ensuring all practitioners can engage meaningfully with digital tools relevant to their roles.
As we look ahead, it becomes clear that a systems-level approach to enhancing digital competencies in public health is vital. Investments in digital infrastructures must parallel workforce training. Public health associations and educational institutions must collaborate to create accessible, targeted training programs that meet diverse needs—especially given generational differences in digital savviness among health workers.
In conclusion, the integration of digital competencies into the training of Canada's public health workforce is not merely an academic exercise; it is essential for adapting to an increasingly complex health landscape. The need for continual evaluation and adaptation of these competencies is crucial in meeting the ever-evolving challenges of contemporary public health. As we strive to build a more informed and technologically adept public health workforce, the call to action is clear: it is time for a transformative approach that equips health professionals with the skills they need to thrive in today's digital age. Will Canada's public health system rise to the challenge of modernization, or will it falter amidst its systemic complexities? The clock is ticking.



 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)