Urgent HIV Prevention: CDC's 2025 Recommendations on Postexposure Prophylaxis
2025-05-09
Author: Wai
Introduction to nPEP
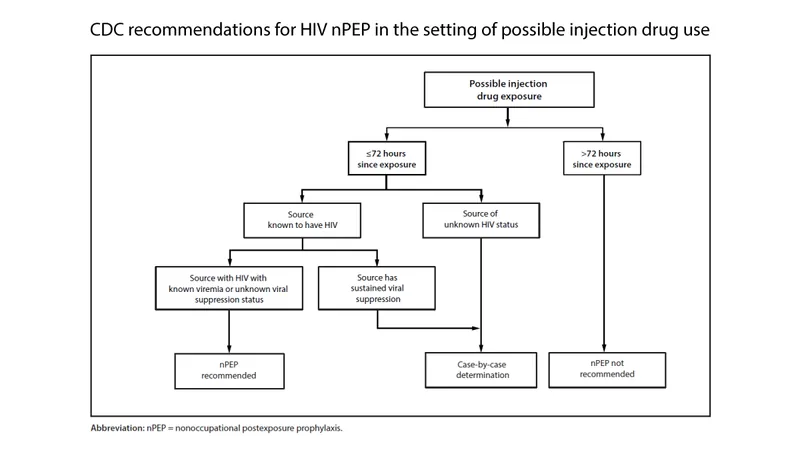
The 2025 CDC guidelines outline essential recommendations for healthcare providers regarding Nonoccupational Postexposure Prophylaxis (nPEP). This can be a critical lifeline for those exposed to HIV through sexual contact, injection drug use, or similar nonoccupational incidents.
When to Use nPEP?
nPEP aims to drastically lower the risk of HIV following significant exposure. The decision hinges on multiple factors, including the HIV status of the source, their viral load, the type of bodily fluid involved, and more. The latest guidance specifies that nPEP is a must if there’s been exposure within the last 72 hours.
Critical Timing for Initiation of nPEP
Time is of the essence! The guidelines push for immediate nPEP initiation, ideally within hours after potential exposure, but definitely within 72 hours. Research indicates that the sooner nPEP is started, the better the chances of preventing HIV infection.
Choosing Your nPEP Medications
A 28-day nPEP course is recommended for those who seek treatment within 72 hours of an exposure. The medications chosen should focus on effectiveness while minimizing side effects to enhance patient adherence.
Monitoring and Follow-Up Care
Labs must be performed at the initiation of nPEP and after the treatment course to monitor kidney and liver health, as well as to test for HIV acquisition. Regular check-ins with healthcare providers throughout the regimen are essential.
Transitioning from nPEP to PrEP
For individuals who continue to face potential HIV exposure, transitioning from nPEP to Pre-exposure Prophylaxis (PrEP) is vital. The CDC emphasizes that PrEP can significantly reduce the risk of HIV if nPEP users anticipate further exposure after completing their course.
Special Considerations for Women and Youth
Pregnant and breastfeeding women should not be deprived of nPEP, and should receive tailored counseling and support. Additionally, the guidelines underscore the importance of addressing the unique needs of children and adolescents when considering nPEP.
Overcoming Barriers to Access
Access to nPEP must be improved. This includes ensuring affordability, timely availability of medications, and education about HIV prevention. Healthcare professionals are urged to support patients in navigating these barriers.
Conclusion
The CDC's 2025 recommendations for nPEP are a beacon for urgent HIV prevention efforts. Quick action, appropriate medication, and continuous healthcare engagement can save lives and prevent new HIV infections.


 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)