Revolutionary Breakthrough in Regenerative Medicine: Human Vision Restored with Stem Cell Therapy!
2024-11-12
Author: Yan
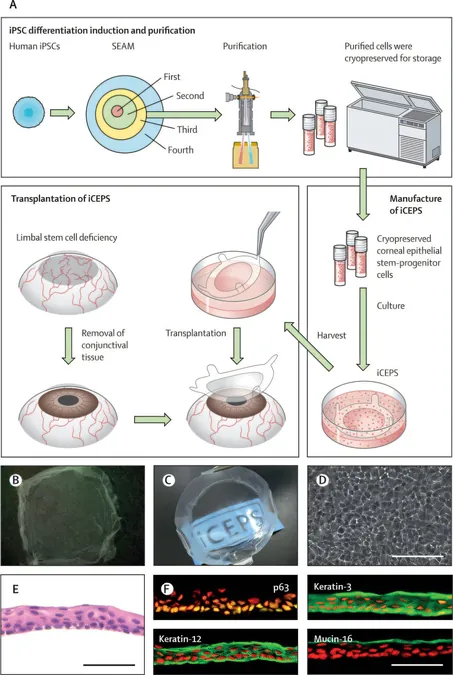
In a groundbreaking advance for vision restoration, researchers from Osaka University in Japan have successfully conducted the first human trial utilizing induced pluripotent stem-cell-derived corneal epithelium for treating limbal stem cell deficiency (LSCD). This innovative approach brings new hope to patients suffering from an ocular condition that can lead to severe vision loss.
LSCD occurs when the limbal stem cells, responsible for regenerating the corneal surface, are compromised. Without these crucial cells, the cornea cannot maintain its transparency and integrity, resulting in the invasion of fibrotic tissue and potential blindness. Conventional treatments often involve using healthy stem cells from the patient's own eye or donors, methods that carry risks of rejection and the loss of healthy tissue.
The study, titled "Induced pluripotent stem-cell-derived corneal epithelium for transplant surgery: a single-arm, open-label, first-in-human interventional study in Japan," was published in The Lancet. It involved the transplantation of pluripotent stem cell-derived corneal epithelial sheets (iCEPS) in four LSCD patients. After carefully excising any fibrotic tissue, the iCEPS were transplanted onto their affected eyes. Remarkably, no HLA matching was required for the transplant surgeries, and half of the participants received low-dose cyclosporine—a drug typically used to prevent organ rejection—while the others were treated with corticosteroids only.
Over a two-year monitoring period, the results were impressive. None of the patients experienced severe complications. Minor issues arose but were effectively addressed without any long-term adverse effects. Most notably, all participants demonstrated significant visual improvements. Three of the four patients transitioned to less severe stages of LSCD, showcasing the promising potential of this treatment. One patient, despite experiencing an initial boost in vision, saw a regression back to baseline after a year due to the severity of their underlying condition.
The studious attention to quality-of-life indicators was equally astounding. Three of the four patients reported enhanced daily living experiences aligned with their visual gains, underlining the profound impact of the treatment beyond just physical restoration.
A critical factor in the success of the iCEPS transplantation was its cultivation technique. This process mimics natural eye development, contributing to graft integrity and minimizing the immunogenic responses that often necessitate stringent HLA matching and prolonged immunosuppression in traditional surgeries. The findings suggest that utilizing low-dose cyclosporine may have provided essential support, hinting at the possible risks associated with not using immunosuppressants.
This successful trial marks a significant milestone in regenerative medicine and ocular therapy, hinting at an exciting future where vision loss could be effectively countered through advanced cellular therapies. Following this achievement, the Osaka University team is gearing up for a larger multicenter trial to solidify these findings and potentially expand the applications of iCEPS transplantation.
Imagine a world where restored vision becomes a reality for those suffering from LSCD. This monumental step forward not only enhances individual lives but could also reshape treatment frameworks for ocular diseases. Stay tuned for more updates as this story continues to unfold!


 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)