Minnesota's Emergency Rooms Overwhelmed as Flu Cases Surge – What You Need to Know!
2025-01-18
Author: Yan
Minnesota's Emergency Rooms in Crisis
Minnesota's emergency rooms are feeling the heat once again, grappling with a surge of patients suffering from influenza and various viral illnesses. This crisis mirrors some of the challenges faced during the peak of the COVID-19 pandemic, forcing hospitals to implement triage systems as a desperate measure to manage overflowing patient numbers.
Innovative Triage Solutions
United Hospital in St. Paul recently adopted a new "split flow" approach designed to expedite patient care even when ER bays are filled to capacity. Just last Thursday, over 20 patients occupied the waiting room, with some receiving IV fluids and others awaiting test results. One particularly frail patient was even accommodated on a hospital bed outside the regular ER setup. Dr. Kelsey Echols, the medical director of the emergency room, noted that this new system allowed for quicker access to care, highlighting its effectiveness even amidst the highest patient volumes the hospital has ever experienced.
Recent Trends in Flu Hospitalizations
The situation saw slight improvement this week as the holiday season came to an end—a peak time notorious for spreading illnesses alongside holiday cheer. A recent state update revealed that flu-related hospitalizations in Minnesota peaked at a staggering 877 in the first week of January but subsequently dropped to 742 in the following week. Nevertheless, these numbers are still historically high, equivalent to the highest recorded figures in the past five flu seasons, stretching hospital resources as they continue to manage patients with COVID-19, RSV, and norovirus infections.
Public Health Recommendations
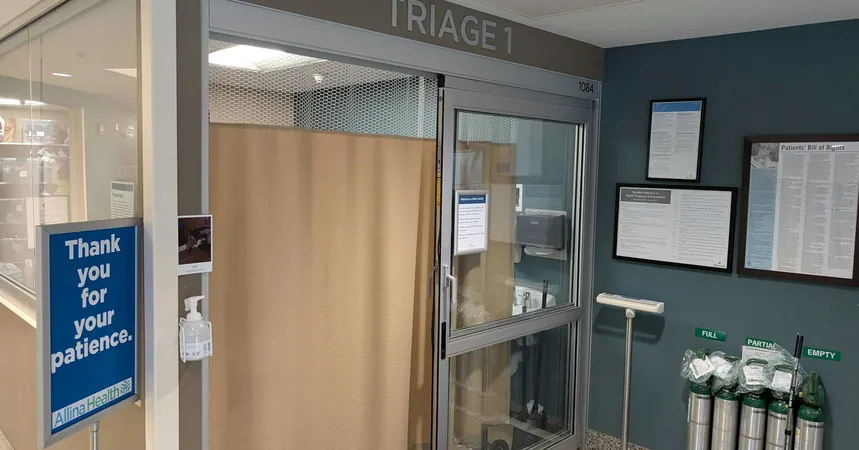
In a bid to protect public health, Dr. Will Nicholson, vice president of medical affairs for M Health Fairview, urged residents to prioritize vaccinations and take preventive measures seriously. Many hospitals, including Fairview's St. John's in Maplewood, have employed the triage strategy to combat incoming patient waves. Allina Health implemented the same tactics at United just last month, having already established protocols in other facilities like Abbott Northwestern Hospital and Mercy Hospital.
Challenges in Emergency Room Operations
Despite the efficiency of the split flow system, the arrival wait time for patients has somewhat stabilized at around 50 minutes; a significant achievement considering the full capacity of 40 ER bays at United. A recent case involving a 72-year-old man named Dave Peterson illustrates the high-stakes environment; although he waited nearly five hours, he still received timely care after being screened and diagnosed with a mild stroke caused by a blood clot.
Patient Backlogs and Long-Term Care Facility Struggles
However, many patients remain in limbo as they await inpatient beds; approximately 30 out of the 40 patients in the ER were stuck on stretchers due to bed shortages. Compounding the issue, outbreaks of influenza were reported in 14 long-term care facilities last week, up from eight the previous week. Such circumstances force nursing homes to operate below capacity due to staff illnesses, exacerbating the backlog of patients waiting to be discharged and reclaiming hospital beds.
Adapting to Growing Demand
In smaller facilities like St. John’s Hospital, which lacks considerable waiting space, the situation becomes even more dire. The hospital had to renovate ER space and create a triage center last year in response to the growing demand, showing just how vital ongoing adaptations are.
Looking Ahead
Nicholson remarked that while triage methods are beneficial, they are merely a temporary stopgap in an ever-evolving healthcare landscape. As the population ages and medical issues become increasingly complex, the strain on emergency services remains ongoing.
The Ongoing Threat of COVID-19
Amid this fluid situation, it’s important to remember that COVID-19 is still a serious concern. The state has reported over 230 COVID-related fatalities since October, predominantly among individuals aged 65 and older. In contrast, flu-related deaths in Minnesota during this timeframe have been significantly lower, totaling 50.
Final Thoughts for Residents
As Minnesota continues to navigate this challenging period, residents are reminded to stay informed and take proactive measures for their health. With the flu season in full swing, adapting to the pressures of a fractured healthcare system has never been more crucial. Stay vigilant, stay healthy, and be prepared for the unexpected!


 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)