Minnesota Hospitals Overwhelmed as COVID, Flu, and Other Viruses Surge!
2025-01-09
Author: Kai
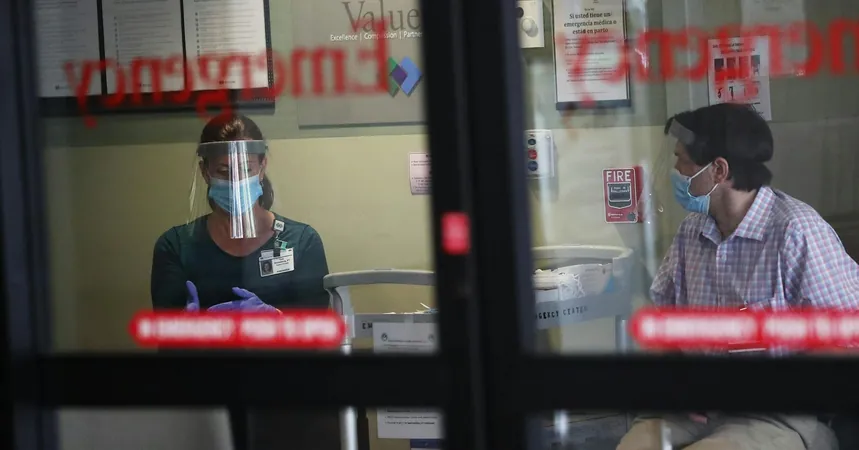
Minnesota is facing a significant healthcare crisis as emergency rooms (ERs) are inundated with patients suffering from a deadly combination of COVID-19, influenza, respiratory syncytial virus (RSV), and norovirus. State health officials warn that the situation is more pressing than it has been since the early days of the pandemic. Recent updates indicated a modest increase in overall COVID-19 cases, but the real concern lies in the alarming rise in flu-related hospitalizations, which have reached levels not previously seen in over five years.
In a shocking revelation, more than 40% of the total 1,763 flu hospitalizations this fall and winter occurred in just one week, underscoring the urgency of the crisis. As a result, Minnesota's risk level for influenza has skyrocketed from low to high, leaving hospitals scrambling for resources.
"We are in a state of crisis," stated Dr. Brandon Trigger, the medical director of the emergency department at M Health Fairview’s Southdale Hospital in Edina. With space running out, patients are being treated in hallways and triage areas, highlighting the extent of the strain on facilities.
Hospital wait times have also soared, with reports indicating a staggering 75-minute wait at St. Mary’s Medical Center in Duluth, while North Memorial Health reports waits of up to 2 hours and 45 minutes in Robbinsdale. In contrast, patients at the Maple Grove facility are experiencing a relatively quicker wait of just 20 minutes. Nevertheless, such variances only add to the uncertainty facing patients in need of care.
In response to the overwhelming demand, metro hospital leaders convened to devise strategies aimed at managing the crowding and ensuring adequate capacity for treating critical conditions such as strokes or heart attacks. “It’s essential that we maintain trauma capacity,” Dr. Rahul Koranne, chief executive of the Minnesota Hospital Association emphasized.
The concurrent rise of multiple respiratory viruses can be attributed partly to the dominance of COVID-19 during the pandemic, which had previously suppressed flu activity. Senior epidemiologist Stephanie Meyer noted that while the pandemic had altered seasonal trends, the pre-holiday surges typical in flu cases are resurfacing with a vengeance.
Allina Health is proactively coordinating among its hospitals to alleviate pressure on the most affected facilities. Dr. Dan O’Laughlin explained that while patient flow can vary greatly between hospitals, the overall picture is one of significant increase in cases.
To maximize available space in the ERs, hospitals, including Southdale, are considering repurposing beds originally intended for surgical and mental health patients. While trauma cases will still receive immediate attention, patients requiring less urgent care may experience longer wait times. “For conditions like appendicitis, patients might wait six to eight hours for a scan,” Dr. Trigger warned.
Healthcare leaders are urging the public to make informed decisions regarding medical care. Family practice physician Dr. Laurel Ries advised, “Only come to the ER if you’re extremely ill; otherwise, consider urgent care or virtual appointments.”
Compounding the problem, flu vaccination rates in Minnesota have fallen below 30%, significantly lower than pre-pandemic levels. This decline, combined with a less effective flu vaccine this season—only reducing hospitalizations by about 35%—has left many at greater risk.
Moreover, long-term care facilities are particularly vulnerable, reporting 17 outbreaks in the past two weeks alone, which may lead to heightened hospitalizations among the most susceptible population: the elderly.
As of yesterday, HCMC reported 294 patients in their care with over 30 waiting for inpatient beds. Dr. Rochelle Zarzar, the senior medical director of emergency services, declared that the downtown hospital has mandated mask-wearing for all personnel in direct contact with patients.
In the midst of this chaos, COVID-19 levels in wastewater have surged to levels not seen since last winter, although COVID-related hospitalizations remain lower than expected. Broader data indicates an increase in visits to Twin Cities ERs for flu-like symptoms, rising from just 1% to over 7% in the past week.
Minnesota's healthcare system faces a pivotal moment. As the battle against multiple concurrent viruses continues, everyone is urged to take precautionary measures, seek timely vaccinations, and choose appropriate medical services to help ease the strain on hospitals. Will this winter spell disaster or resilience for Minnesota's healthcare system? Only time will tell.




 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)