Minnesota Emergency Rooms Overflow as Flu Season Hits Historic Highs: What You Need to Know!
2025-01-19
Author: Wai
Overview of the Situation
Minnesota's emergency rooms are facing unprecedented challenges as a surge in influenza and other viral illnesses strains hospital resources. With the flu epidemic reaching staggering levels, hospitals are once again relying on triage systems, initially implemented during the COVID-19 pandemic, to manage the influx of patients.
Innovative Approaches in Care
Recently, United Hospital in St. Paul adopted a "split flow" approach to expedite care. This innovative method allows medical staff to begin treatment for patients right in the waiting area, a necessary adjustment given the overwhelming number of individuals seeking care. On a busy Thursday afternoon, over 20 patients were crammed into the waiting area, some receiving intravenous fluids while others awaited crucial lab results. Dr. Kelsey Echols, the hospital's emergency medicine director, shared her personal battle with the flu, emphasizing the importance of prompt care even amid record-high patient volumes.
Trends in Hospitalizations
After the holiday season, there seems to be a slight decline in flu-related hospitalizations. Data shows that hospitalizations peaked at 877 in early January but dropped to 742 by mid-January—still the highest figures reported in the past five flu seasons. Hospitals continue to juggle co-existing outbreaks of COVID-19, RSV, and norovirus, placing immense pressure on healthcare systems.
Health Precautions
Healthcare professionals, including Dr. Will Nicholson from M Health Fairview, are urging the public to take preventive measures. "Take care of yourself, folks," he cautioned, emphasizing the importance of vaccinations, staying home when under the weather, and other safety precautions.
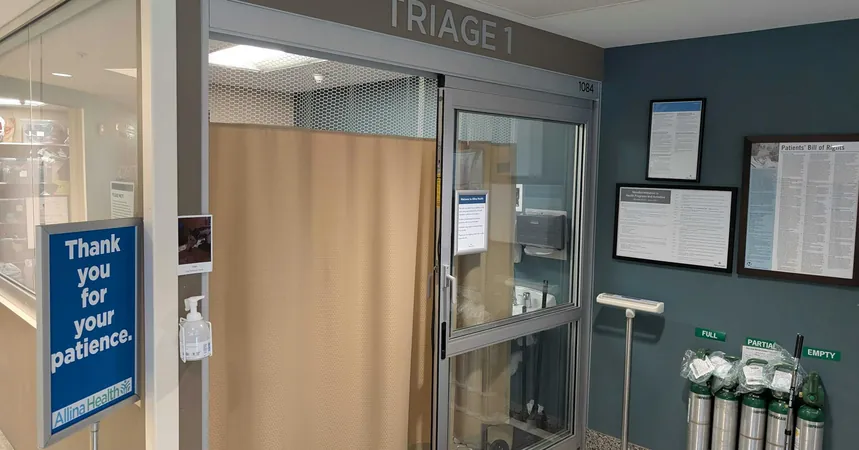
Triage Protocols Implemented
Additionally, various hospitals, including those part of Allina Health, have implemented triage protocols in anticipation of this flu surge. For example, at St. John's Hospital in Maplewood, patients were tended to based on the severity of their conditions, effectively reducing wait times.
Challenges with ER Congestion
However, the sheer volume of patients—40 ER bays were occupied at United Hospital on notable days—remains alarming, and the wait time for new arrivals stretched to about 50 minutes. While some patients, like 72-year-old Dave Peterson, achieved timely care through the triage system, many others faced long waits. Peterson's case illustrates a critical point: those awaiting inpatient beds significantly contribute to ER congestion.
Impact on Long-term Care Facilities
The situation is exacerbated by ongoing flu outbreaks in long-term care facilities. Reports indicate a surge from eight outbreaks in the previous week to 14, which leads to staffing shortages; thus, hospitals struggle to discharge patients to make room for new arrivals.
Conclusion
Dr. Nicholson acknowledges that while triage care provides an immediate solution, it’s only part of the answer. Smaller hospitals, such as St. John's, have struggled with overflow issues, even renovating spaces into triage centers to alleviate pressure. Amidst this turmoil, COVID-19 still lurks as a threat, although hospitalizations have decreased compared to last year. Recent wastewater samples suggest that COVID-19 levels peaked in early January, leading to expectations of a decline in related hospitalizations. While the immediate threat from COVID-19 seems to be less intense, it still accounts for over 230 deaths since October, predominantly among older individuals.


 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)