Is America Facing a Crisis of Confidence in Public Health? Renowned Doctor Reveals Shocking Insights!
2024-09-24
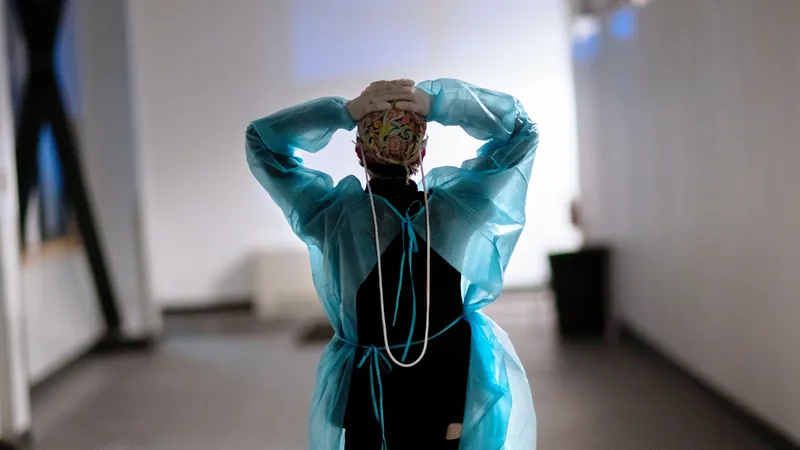
The Rise of Mistrust
Dr. Makary highlighted a growing 'epidemic of mistrust' in public health, particularly as people reevaluated the advice they received throughout the pandemic. He pointed out that many who challenged the mainstream narratives—such as concerns about lengthy school closures, mask mandates for toddlers, the validity of natural immunity, and the implications of COVID vaccine boosters—were ultimately successful in asserting their positions.
One of the most distressing public health decisions during this time, according to Dr. Makary, was the prohibition of visitations for individuals in hospitals who were suffering from terminal illnesses. "That was a human rights violation," he asserted. "No one should be barred from comforting their dying loved one, regardless of circumstance."
More Than Just COVID-19 Errors
Dr. Makary warns that the mistakes made during the COVID-19 crisis represent merely the surface of deeper issues within public health guidance. His book, *Blind Spots: When Medicine Gets It Wrong, and What It Means for Our Health*, recounts several historical missteps, including the now-discredited advice to keep peanut products away from young children, which some believe ignited the current peanut allergy epidemic. Furthermore, he noted that the opioid crisis was fueled by a widespread belief that prescription opioids could be safely administered without the risk of addiction.
He also criticized the USDA's Food Guide Pyramid, which dominated dietary recommendations for over a decade. "These guidelines may have contributed to the rise in obesity and diabetes, quintessentially linked to the processed foods pushed by the food industry," he explained.
The Faulty Mindset of Medical Experts
The crux of Dr. Makary's argument revolves around the entrenched patterns of thinking that can pervade the medical field. He believes that rather than grounded in scientific evidence, many health recommendations arise from collective biases and assumptions entrenched over time. This is reflected in how a significant portion of healthcare professionals dismiss hormone replacement therapy for older women, echoing a dated stance that lacks current scientific support.
"Such intellectual laziness can lead to misguided decisions in patient care, where doctors continue to overprescribe antibiotics despite emerging evidence showing their negative impact on gut health," he warned.
Re-evaluating Beliefs
Dr. Makary encourages both health professionals and the general public to critically examine their beliefs, questioning if they are based on solid evidence rather than mere tradition or initial assumptions. He argues that this scrutiny should extend to how we treat chronic conditions, advocating for lifestyle and dietary changes instead of an over-reliance on medications.
“We need a paradigm shift," he urged, "to consider environmental factors in disease management and not solely rely on pharmaceuticals. Education on nutrition and wellness should play a much more significant role."
A Caution Against Overreaction
While Dr. Makary is unequivocally critical of public health failures, he also warns against a blanket distrust of all medical professionals. "In emergencies, trust your doctor. But in non-urgent matters, it’s perfectly acceptable to question and explore alternative treatments," he advised.
He advocates for a more transparent healthcare dialogue where doctors can candidly acknowledge their knowledge limits, particularly in complex cases like chronic pain or the increasing rates of autism.
Return to Traditional Wisdom
Dr. Makary posits that many of our chronic health issues could benefit from a return to more traditional ways of living. He points to ancient health principles that emphasize whole foods and community well-being, alongside practices like fasting and prayer, as being beneficial for mental and physical health.
In a rapidly changing world of public health guidance, having open, inquisitive conversations—and looking back at time-tested practices—could guide Americans towards better health outcomes.
Conclusion
In summary, as public trust in health authorities wanes, it's crucial to remain informed and question health narratives with both skepticism and an open mind. Could a fresh approach, one rooted in evidence and tradition, rebuild the bridge between patients and healthcare professionals? Only time—and further dialogue—will tell.



 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)