Essential CDC Guidelines for HIV Post-Exposure Prophylaxis (PEP) in 2025
2025-05-08
Author: Chun
Critical Recommendations for Clinicians
The CDC has outlined crucial guidelines for healthcare providers regarding nonoccupational post-exposure prophylaxis (nPEP) for HIV. These recommendations cover everything from patient evaluation to therapy completion, emphasizing the need for swift action and tailored treatment strategies.
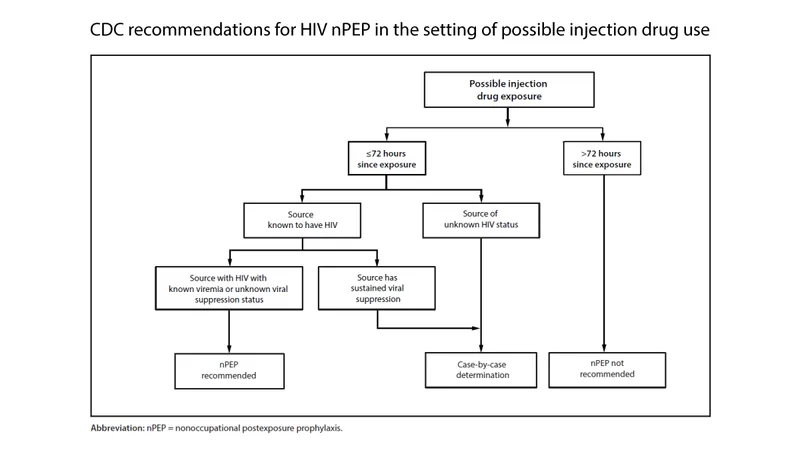
Understanding When to Implement nPEP
HIV nPEP is a preventive treatment aimed at reducing the risk of HIV infection after potential exposure, such as through sexual contact or injection drug use. Factors influencing the decision to administer nPEP include the HIV status of the source, the timing of the exposure, and the presence of viral suppression.
Timing is Everything: The 72-Hour Rule
Initiating nPEP within 72 hours of exposure is essential. Research indicates that the sooner treatment is started, the higher the chances of preventing HIV infection. Healthcare providers are urged to act decisively without waiting for complete laboratory results.
Choosing the Right Regimen
The recommended nPEP regimens for adults include a combination of two nucleoside reverse transcriptase inhibitors (NRTIs) with a second-generation integrase strand transfer inhibitor (INSTI). Patient tolerance and ease of adherence are priorities, with a 28-day course being the standard treatment duration.
Laboratory Testing and Follow-Up Care
At the first appointment, patients should undergo laboratory testing to ensure they do not have pre-existing HIV. Follow-up tests are crucial at 4-6 weeks and 12 weeks post-exposure to monitor for possible infection.
Supporting Vulnerable Populations
nPEP should be made readily available to vulnerable populations, including survivors of sexual assault and pregnant or breastfeeding women. A trauma-informed approach is encouraged to ensure these individuals receive appropriate care.
Transitioning to Pre-Exposure Prophylaxis (PrEP)
After completing an nPEP regimen, individuals at continuing risk for HIV should be transitioned to PrEP, which can significantly reduce the likelihood of future infections. Immediate referral is advised for those needing ongoing protection.
Confronting Barriers to Access
Healthcare systems should address socio-economic barriers that may hinder access to nPEP. Innovative delivery strategies, such as 'PEP-in-pocket' programs, could provide essential medications directly to those at risk.
Conclusion: Empowering Healthcare Providers
By adhering to these updated CDC guidelines, healthcare providers can play a pivotal role in reducing the incidence of HIV, ensuring timely care, and supporting vulnerable populations in crisis.



 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)