Unveiling the Truth: Do Vaccinations Increase the Risk of Rheumatoid Arthritis? Updated Meta-Analysis of Nearly 26 Million Participants Reveals Surprising Findings!
2025-03-10
Author: Charlotte
Introduction
Rheumatoid arthritis (RA) is a chronic autoimmune disorder characterized by inflammation of the joints and surrounding tissues. Concerns have arisen linking vaccinations to a heightened risk of developing RA, prompting extensive research in this area. A new systematic review and meta-analysis, aggregating data from an astonishing 25,949,597 individuals, has sought to clarify these concerns.
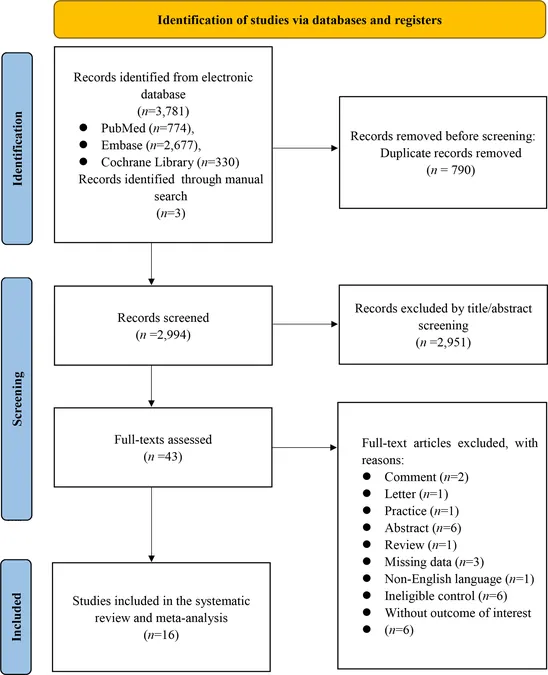
Methodology
The researchers conducted a meticulous search spanning PubMed, EMBASE, and the Cochrane Library for relevant cohort and case-control studies from inception through September 2024. Utilizing the Newcastle-Ottawa Scale for bias assessment and employing the GRADE system for evidence appraisal, the team utilized STATA software for statistical analyses, focusing on relative risk (RR) and confidence intervals (CI).
Results Summary
Sixteen observational studies from 2008 to 2024 were included, representing diverse populations and a wide range of vaccination types. The analysis revealed no significant association between vaccination and RA risk, with a relative risk of 1.03 (95% CI 0.95–1.11). Subgroup analyses on HPV, influenza, anthrax, herpes zoster, and COVID-19 vaccinations did not provide evidence of a significant risk increase. Interestingly, a subgroup analysis for individuals with follow-up durations between 0.5 to 1.8 years indicated a protective effect of vaccinations for HPV and COVID-19, suggesting an RR of 0.92 (95% CI 0.87–0.98).
Conclusions
The findings challenge earlier assumptions linking vaccinations and RA risk, indicating insufficient evidence to suggest vaccinations contribute to RA development. Moreover, there seems to be a potential protective aspect of vaccinations against RA during shorter follow-up periods, emphasizing the need for more refined and comprehensive future studies focusing on RA and vaccination ramifications.
Implications and Future Directions
Despite the compelling sample size and rigorous methodology, the study emphasizes the necessity for ongoing research. Future studies should delve deeper into specific populations, assess diverse types of vaccines separately, and include different demographic factors, particularly given the variability and limitations observed in existing research. Engaging populations with distinct epidemiological profiles, such as those in Africa with high infectious disease burdens, could bring new insights into vaccine-associated risks or benefits with respect to RA.
Final Thoughts
As the medical community continues to navigate the complexities of autoimmune disorders and their potential relationships with vaccinations, understanding the underlying mechanisms of these interactions remains critical. While this meta-analysis offers a beacon of clarity, the journey of exploration into the safety and impact of vaccinations on conditions like RA is far from over, with significant implications for clinical practice and public health policies.








 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)