Unraveling the Intricate Links: How Mental Disorders Influence Frailty - A Groundbreaking Study Reveals Shocking Insights!
2024-12-23
Author: Michael
Introduction
In recent years, the growing awareness of health issues has shone a spotlight on frailty, a condition linked to numerous adverse health outcomes. Defined by Fried et al. in 2001, frailty comprises various syndromes characterized by decreased functionality due to diminished muscle mass, nutritional deficiencies, hormonal fluctuations, and heightened inflammation. With the aging global population, the prevalence of frailty is set to escalate.
Study Overview
A recent study by a team of researchers, encompassing a robust sample of 5,844 elderly individuals across diverse urban areas, reported a frailty prevalence of 9.9%. This aligns with other surveys indicating that approximately 10.7% of older adults living independently are frail. The prevalence of frailty varies significantly, reported estimates range from 4% to 59.1%, reflecting differences in measurement methodologies.
Current Assessments
Current frailty assessments predominantly involve the frailty phenotype (FP) and the frailty index (FI). The FP identifies a clinical syndrome based on five manifestations: fatigue, weakness, slow walking speed, unintentional weight loss, and low physical activity. Concurrent conditions, including depression, often present overlapping symptoms, complicating diagnosis. Conversely, the FI is calculated based on the cumulative count of health deficits over time, providing a more comprehensive overview of an individual’s health status.
Mental Disorders and Frailty
Emerging evidence reveals a substantial correlation between mental disorders and physical frailty. For instance, a study involving 315 elderly outpatients found significantly higher frailty rates among individuals with varying levels of depression: 14.5% in non-depressed individuals skyrocketed to 65.1% in those severely depressed. Moreover, research suggests that individuals experiencing conditions such as insomnia, schizophrenia, and bipolar disorder are more likely to exhibit signs of frailty.
Bidirectional Relationship
Intriguingly, the relationship between mental disorders and frailty may be bidirectional. Existing studies have indicated that not only do mental disorders increase the risk of frailty, but frailty itself can exacerbate mental health issues. However, most existing literature relies on cross-sectional analyses, leaving the causal relationships unclear.
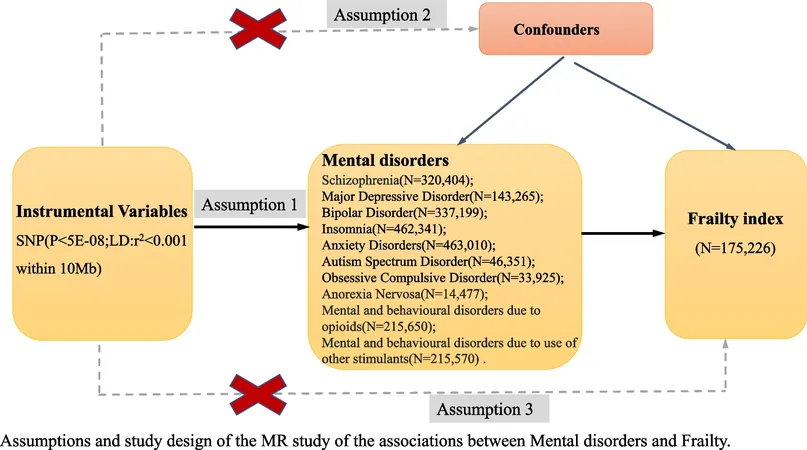
Mendelian Randomization Study
To address this gap, researchers conducted a comprehensive Mendelian randomization (MR) analysis—a genetic study methodology that uses genetic variations as instruments to determine causal effects. In their study, they focused on ten common mental disorders, including schizophrenia, major depressive disorder, bipolar disorder, and insomnia, analyzing their genetic influences on frailty.
Key Findings
The results were illuminating. A statistically significant causal link was discovered between genetically predicted major depressive disorder and frailty, with an odds ratio indicating a clear association. Schizophrenia also exhibited a causal effect on frailty, though no significant correlation with the other mental disorders was detected.
Implications of the Findings
These findings have profound implications; as major depressive disorder affects over 264 million people globally, understanding its link with frailty underscores the importance of integrated health management. Additionally, addressing mental disorders can be crucial in preventing the onset or exacerbation of frailty, particularly among the aging population.
Limitations of the Study
However, the study has limitations. It primarily involved participants of European ancestry, prompting caution in generalizing results to other ethnic groups. Notably, the research lacks sufficient genetic data for certain mental disorders like obsessive-compulsive disorder, indicating an area ripe for further inquiry.
Future Directions and Conclusion
The study invites a deeper exploration into how interventional strategies targeting mental health could potentially mitigate the frailty epidemic. With the potential for frailty to serve as a reversible variable, creating a pathway for health workers to implement preventative and therapeutic measures becomes crucial. Thus, ongoing research in this intriguing field is essential to unravel the complexities of mental health and frailty—a challenge that has far-reaching implications for public health policy and education. Stay tuned as we continue to monitor this developing story because these revelations could transform how we approach mental health in connection with physical well-being!








 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)