Unraveling Insomnia in Chronic Schizophrenia: The Hidden Links between Symptoms, Inflammation, and Lipid Metabolism
2025-08-28
Author: William
A Deep Dive into Schizophrenia and Insomnia
Schizophrenia, a severe mental disorder characterized by cognitive dysfunction and distorted perceptions, affects many worldwide, with a lifetime prevalence of 0.7% in China alone. One of the most debilitating symptoms faced by these patients is insomnia, impacting up to 80% of the population at various stages of the disorder. This study aims to illuminate the intertwined relationships between insomnia and schizophrenia's clinical features, lipid metabolism, and inflammation.
Insomnia: A Symptom of Serious Concern
Research highlights a staggering rate of insomnia among schizophrenia patients, with nearly half experiencing significant sleep disturbances. Insomnia not only manifests as a primary concern but exacerbates other clinical symptoms, contributing to cognitive decline and elevating the risk of suicide. Understanding the risk factors linked to insomnia in schizophrenia is crucial for improving patient outcomes.
The Psychotic Link: How Symptoms Propel Insomnia
Insomnia symptoms are intricately correlated with psychotic symptoms. Recent analyses show a strong linkage between hallucinations and sleep disturbances, where heightened psychotic features may worsen insomnia. This bi-directional relationship indicates that while psychotic symptoms can initiate sleep issues, the reverse is also true, creating a cycle that detrimentally affects mental health.
The Impact of Depression on Sleep
Depression is a frequent companion to schizophrenia, affecting about 28.6% of patients. This depressive state profoundly disrupts sleep quality, reinforcing the need for healthcare providers to assess and treat depressive symptoms as a vital step in tackling insomnia.
The Role of Metabolism and Inflammation
Schizophrenia patients often struggle with metabolic dysregulation, which can severely impact sleep quality. Notably, inflammatory markers like IL-6 may herald increased insomnia risk, hinting at an intertwining of mental health, metabolic health, and inflammation. Understanding the biochemical landscape in these patients opens avenues for tailored interventions.
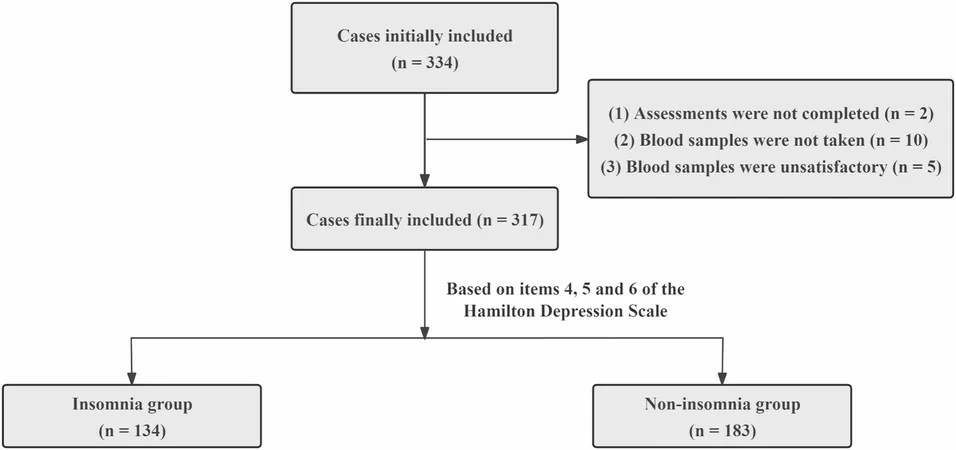
Study Overview: Participants and Methods
Conducted across several hospitals in Anhui Province, this cross-sectional study involved 317 patients diagnosed with chronic schizophrenia. Among other measures, researchers evaluated insomnia symptoms via the Hamilton Depression Rating Scale and psychotic symptoms using the PANSS. Blood samples were collected to analyze inflammatory cytokines and lipid metabolism markers.
Key Findings: A Closer Look at Insomnia Prevalence
The study revealed that 42.3% of chronic schizophrenia patients experience insomnia. Significant correlations emerged between insomnia and factors such as age, higher positive symptom scores, and elevated IL-6 levels, highlighting the importance of these variables in both research and treatment contexts.
The Importance of Comprehensive Assessment
Given the multifaceted nature of insomnia in schizophrenia, a holistic approach that considers emotional, clinical, and biochemical factors is essential. This includes looking beyond traditional clinical variables to include biomarkers such as inflammatory and lipid metabolism markers.
Future Directions and Implications
While this study marks a step toward understanding insomnia's complexities in schizophrenia, future research should aim for larger, longitudinal designs to forge clearer causal links. As the relationship between inflammation, metabolism, and sleep disturbances unfolds, targeted therapies could revolutionize care for those suffering from chronic schizophrenia.








 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)