The Surprising Link Between H. pylori and Inflammatory Bowel Disease Severity Revealed!
2025-04-29
Author: Liam
Understanding Inflammatory Bowel Disease (IBD) and H. pylori
Inflammatory bowel disease (IBD) encompasses Crohn’s disease (CD) and ulcerative colitis (UC), conditions marked by unpredictable flare-ups and periods of remission. These chronic diseases require careful management to avert serious complications. Research indicates that genetics and environmental factors intertwine to influence IBD development, making it critical to tailor treatment plans for individual patients.
Is H. pylori Friend or Foe?
A key focus in gastroenterology is the connection between Helicobacter pylori (H. pylori) and IBD. Studies yield conflicting results about how prevalent this bacteria is among IBD patients and its influence on disease severity. Some case-control investigations have shown that UC patients have lower rates of H. pylori infection, hinting at a possible protective effect against the disease.
Intriguingly, while many studies propose that H. pylori might shield against IBD, others have found no conclusive link. A recent study aimed to uncover these relationships specifically in Saudi Arabia and the Gulf region, areas previously unexamined for H. pylori prevalence in IBD.
Research Findings: A Closer Look
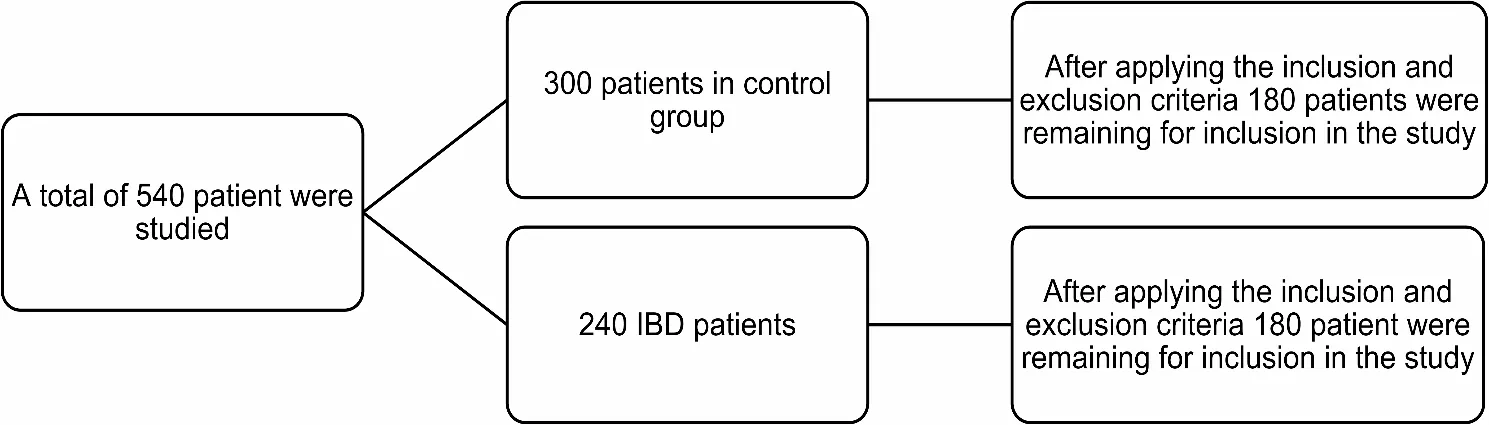
The study involved 360 participants, evenly split between an IBD group and a control group. Among IBD patients, Crohn's disease had 91 cases, and ulcerative colitis had 89 cases. Shockingly, only 13.9% of IBD patients had H. pylori compared to 23.3% in the control group. Interestingly, autoimmune diseases appeared more frequently in the control group than among IBD patients.
H. pylori Infection and Lifestyle Factors
Further analysis revealed that H. pylori infection was significantly less common among non-smokers compared to smokers in the IBD group. Current smokers had a much higher prevalence of H. pylori infection, raising questions about lifestyle factors' role in disease progression.
Activity Scores and Treatment Implications
In evaluating disease activity, patients with H. pylori and those without showed similar remission rates, with slightly more severe cases in the H. pylori-negative group, though these differences were not statistically significant. Furthermore, the research found no substantial connection between H. pylori infection and medication use among IBD patients, indicating that treatment strategies remained unaffected by the presence of this bacteria.
Conclusion: What Does This Mean for IBD Patients?
This study underscores the perplexing nature of H. pylori infection and its ambiguous relationship with IBD severity. With more research needed to untangle these complex interactions, it’s clear that while H. pylori might offer some protective effects, the implications on treatment strategies, disease severity, and the role of lifestyle factors such as smoking remain crucial areas for further investigation.
A Call for More Research!
As scientists continue to navigate the intricate ties between H. pylori and IBD, patients and healthcare providers alike must remain vigilant and informed. The ongoing exploration of these connections may lead to breakthroughs in how we understand and treat not just IBD, but perhaps other related gastrointestinal conditions.






 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)