The Silent Killer: Brainworms Devastating Moose Populations Across America
2025-09-21
Author: Emily
The Tragic Tale of a Moose on the Road
Imagine a moose in Minnesota, lost and disoriented, stumbling onto a busy road. Oblivious to the danger of an approaching semitruck, she’s met with a horrific fate. Yet, what truly causes her demise isn’t just the tragic collision, but a sinister brainworm lurking within her head.
What is the Brainworm?
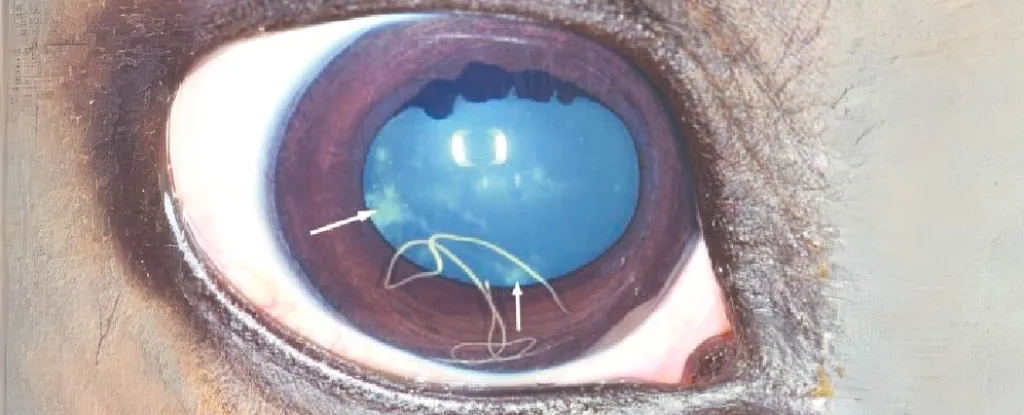
Known scientifically as Parelaphostrongylus tenuis, this parasite is a deadly nematode that targets a wide range of herbivores, particularly moose and elk. Once inside its unsuspecting host, it can wreak havoc, leading to severe neurological disorders and, often, death.
The Dire Consequences of Infection
While the story of the Minnesota moose is fictional, the reality is chilling. This brainworm has been responsible for catastrophic neurological impairment in many wild animals, causing symptoms such as confusion, circling, paralysis, and eventually death. For wildlife managers, understanding and tracking the spread of this parasite is crucial for protecting moose populations.
The Intricate Life Cycle of the Brainworm
The disease’s cycle begins with white-tailed deer, which can carry the parasite without showing any symptoms. When these deer defecate, they release the larvae into their environment, which can then be ingested by snails and slugs. These creatures serve as intermediate hosts, allowing the worm to develop further and eventually infect other ungulates like moose and elk.
Spotting the Enemy Before It's Too Late
One major challenge for researchers is detecting the disease early enough to prevent irreversible damage. Since only white-tailed deer excrete the parasite, fecal analysis from moose or other animals is ineffective. By the time an infected animal shows visible signs of illness, recovery is typically impossible.
Complicated Diagnoses and Misidentifications
To complicate matters further, symptoms of brainworm infection can be confused with those caused by other parasites, such as the arterial worm. Distinguishing between the two is crucial because differing mitigation strategies are required for each. Accurate diagnosis often hinges on genetic analysis for definitive identification.
A Breakthrough in Diagnostics
Fortunately, collaborators at the University of Tennessee have developed a groundbreaking serological test. This test can detect antibodies in the blood of affected moose or elk, allowing for earlier diagnosis while the animals are still alive. Samples collected from sick or deceased animals are shipped for analysis, leading to quicker responses to outbreaks.
The Ripple Effect of Testing
In our hypothetical scenario, after a moose is struck by a truck, wildlife officials collect a blood sample before the body is processed. This sample may join thousands from across North America, helping scientists refine their testing methods. Positive results from areas previously unexposed to the brainworm may alert biologists to the expanding range of the parasite, enabling preemptive action.
Taking Action Against the Parasite
When early detection occurs, wildlife managers have time to implement strategies such as controlling snail populations or adjusting hunting regulations for white-tailed deer to reduce the risk of disease spread. This proactive approach is essential for protecting both moose and the ecosystems they inhabit.
A Hopeful Future for Moose Populations
With these advancements in testing and tracking, we hope to create frameworks that other researchers can use against various infectious agents. The fight against the brainworm isn’t just about saving individual moose, but about preserving the delicate balance of North America's wildlife.






 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)