The Hidden Danger: How Delayed Hospital Admission Increases Risk of Deep Vein Thrombosis in Hip Fracture Patients
2025-04-05
Author: Jacques
Objective:
This study aims to shed light on a critical health issue: the relationship between deep vein thrombosis (DVT) in the lower limbs at the time of hospital admission and the time elapsed from the injury to hospital admission (TFITA). Such insights could be pivotal for improving clinical methods to prevent DVT in vulnerable hip fracture patients.
Study Overview:
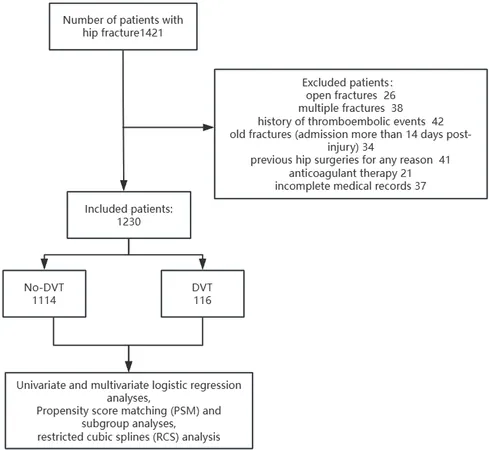
The research drew data from patients admitted for hip fractures over a six-year span from January 2017 to December 2023. It employed both univariable and multivariable logistic regression analyses to gauge the connection between TFITA and DVT at admission, while also utilizing advanced statistical techniques like propensity score matching (PSM) and restricted cubic splines (RCS) analysis to strengthen the findings.
Key Findings:
A total of 1230 patients were analyzed, revealing that those with DVT at the time of admission had a longer TFITA—averaging 40 hours—compared to 20 hours for those without DVT. This study confirmed a significant positive correlation between extended TFITA and higher rates of DVT occurrence at admission, underlining the urgency of timely medical intervention.
In fact, each additional hour of delay in admission increased DVT risk steadily, affirming that a TFITA of 36 hours served as a key threshold. The results showed that patients with a TFITA of 36 hours or longer were almost 2.4 times more likely to develop DVT.
Why This Matters:
Hip fractures are unfortunately common among the elderly, significantly increasing the likelihood of complications such as DVT due to prolonged immobility. DVT itself can lead to severe consequences, including chronic pain, pulmonary embolism (PE), and long-term disabilities, which can dramatically affect patients' quality of life.
Statistical evidence indicates that patients with hip fractures facing a delay of more than two days in being admitted can see their risk of developing preoperative DVT soar to 54%. Researchers concluded that constructors of clinical pathways must prioritize reducing TFITA to mitigate these risks.
Clinical Insights:
Timely admission can profoundly decrease DVT incidence, and this study advances the rationale for immediate evaluation and intervention strategies for patients with hip fractures. Using risk stratification tools like the Wells score can enable early identification and even prompt prophylactic treatment strategies including anticoagulants and mechanical compression devices.
Furthermore, the importance of addressing systemic inflammation that arises with hip fractures cannot be overstated. Early admission allows for better management of this inflammation, which is linked to the increased clotting tendencies that contribute to DVT.
Conclusion:
As the incidence of hip fractures continues to rise with an aging population, understanding the associations between TFITA and DVT is imperative. This research not only highlights a critical preventive measure but also serves as a call to action for healthcare providers: swift admission is essential for lowering the risk of life-altering complications associated with DVT. Future studies can build upon these findings to explore the broader implications of TFITA in various trauma settings, significantly enhancing patient care and outcomes.
Overall, this investigation underscores the pressing need for healthcare systems to streamline admission processes and implement targeted DVT prevention strategies in hip fracture patients—potentially saving lives and improving health outcomes across the spectrum.









 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)