The Alarming Rise of Hyperactive Delirium in Elderly Hospital Patients: Uncovering Risk Factors and Outcomes
2025-04-03
Author: Sophie
Introduction
In a groundbreaking prospective cohort study, researchers delved into the silent yet alarming rise of hyperactive delirium among older medical inpatients admitted to non-intensive care units (non-ICU) at Ramathibodi Hospital, Mahidol University, in Thailand. The study aims to highlight the pressing issue of hyperactive delirium, a condition often overlooked, shedding light on its significant impact on patient outcomes including unexpected rehospitalizations, emergency department (ED) visits, and mortality rates.
Study Overview
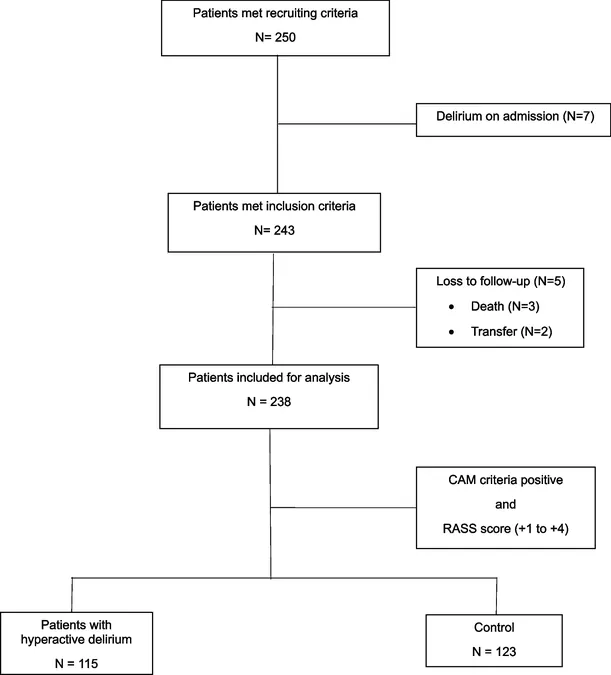
Conducted over a 16-month period from September 2022 to December 2023, this prospective observational study closely monitored 238 older medical patients, all aged 60 and above, admitted to non-ICU settings. The study hypothesized that hyperactive delirium would correlate with adverse outcomes post-discharge. Trained medical staff recorded daily conditions of the patients, identifying 115 individuals who experienced hyperactive delirium.
What is Hyperactive Delirium?
Hyperactive delirium is characterized by heightened levels of agitation, restlessness, and aggressive behavior, making it essential for healthcare teams to recognize and treat it promptly. The condition could lead to severe complications if not identified early, including increased mortality rates. The study used the Confusion Assessment Method (CAM) and the Richmond Agitation-Sedation Scale (RASS) to diagnose this condition.
Key Findings
1. **Prevalence:** An astonishing 48.3% of the older patients developed hyperactive delirium during their hospital stay. 2. **Risk Factors Identified:** Key risk factors for hyperactive delirium included cognitive impairment, as indicated by low scores on the Montreal Cognitive Assessment (MoCA), frailty, assessed using the Clinical Frailty Scale (CFS), and urinary incontinence. 3. **90-Day Outcomes:** Patients with hyperactive delirium faced a staggering eightfold increase in the risk of all-cause mortality within 90 days of discharge compared to their peers without delirium. The mortality rate in the delirium group was reported at 12.2%, compared to only 1.6% for those without. 4. **Impact on Healthcare:** The study revealed that patients with hyperactive delirium had longer hospital stays and were more frequently prescribed high-risk medications contributing to delayed recovery.
Implications for Healthcare
This study serves as a clarion call for healthcare professionals to refine monitoring strategies and enhance communication regarding the risks associated with hyperactive delirium in older patients. It emphasizes the need for comprehensive medication reviews to minimize polypharmacy and optimize treatment plans—ensuring patient safety and improving long-term health outcomes.
Conclusion
The findings underscore the urgent need for proactive measures in preventing and managing hyperactive delirium among older inpatients. By identifying high-risk patients early and implementing targeted interventions, healthcare providers can significantly reduce the burden of adverse outcomes linked to this debilitating condition. Future research should continue exploring innovative strategies to mitigate these risks, which may include training staff on early detection of delirium and better assessment protocols. This research not only fills a crucial gap in our understanding of hyperactive delirium but also serves as a blueprint for improving clinical practices to enhance the care of the elderly population within healthcare systems worldwide.








 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)