Shocking Links Between Insomnia and Suicide Attempts in Schizophrenia Patients with Autism Symptoms
2025-07-01
Author: Benjamin
Understanding the Dark Side of Schizophrenia
Schizophrenia (SCZ) is a severe mental disorder that disrupts a person’s thoughts, emotions, and behaviors. Classified among the most debilitating mental health issues, SCZ can dramatically shorten a patient’s life expectancy by about a decade, with suicide emerging as the leading cause of this tragic outcome. Studies reveal that individuals with chronic SCZ are at an increased risk of suicidal behavior, fueled by a complex interplay of factors.
The Insomnia Epidemic
Insomnia is alarmingly prevalent among SCZ patients, affecting between 25% to 50% of individuals. This persistent inability to sleep can stem from various causes, including dysfunction in the body’s internal clock. Polysomnographic studies show that SCZ patients struggle with prolonged sleep initiation and reduced rapid eye movement (REM) sleep, both of which can exacerbate mental health issues.
Unraveling the Suicide Puzzle
Research shows a strong correlation between insomnia and increased suicidal thoughts and attempts. Patients grappling with SCZ who also experience insomnia report twice the likelihood of contemplating or attempting suicide as compared to their well-rested peers. Despite previous studies highlighting this connection, some have found no significant association, leading to debates about the role of ethnicity, genetics, and the disease's progression in these outcomes.
Autism Symptoms: A Double-Edged Sword
Emerging evidence indicates a significant relationship between autism symptoms (AS) and SCZ, complicating the clinical picture. While patients with AS often exhibit fewer suicidal thoughts, they also struggle with social interactions, communication, and repetitive behaviors. Notably, those with AS generally score lower on cognitive tests, possibly diminishing their suicide risk compared to other SCZ patients.
A New Study Sets the Stage
A groundbreaking study involving 955 Chinese Han patients with chronic SCZ sheds light on the relationship between insomnia and suicide attempts, particularly among those with AS. The researchers hypothesized that insomnia would correlate with an increased risk of suicide attempts, moderated by the presence of autism symptoms.
Key Findings
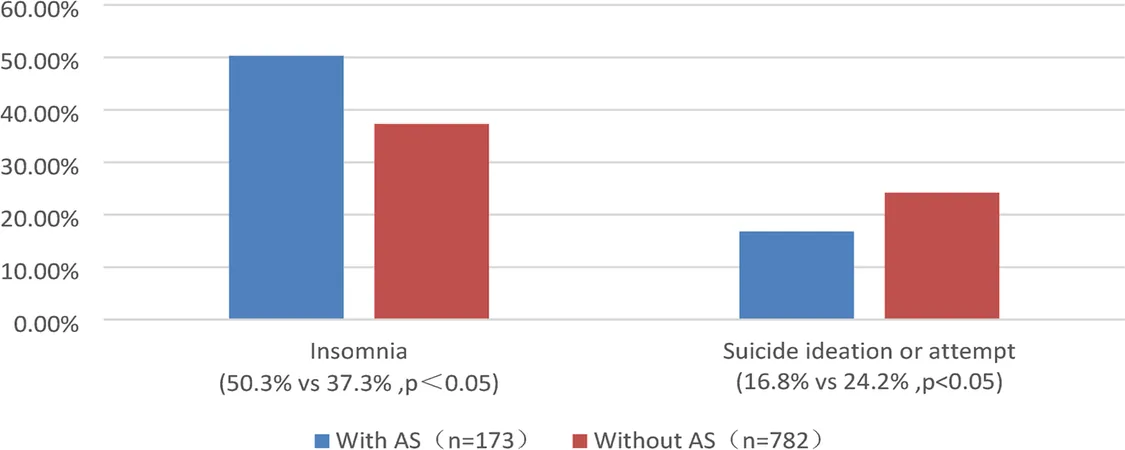
The study revealed that 39.7% of SCZ patients suffered from insomnia, a figure in line with previous research. However, the incidence of insomnia was significantly higher among SCZ patients with AS. This finding opens new discussions about the unique challenges faced by SCZ patients with autism traits and highlights the urgent need for tailored interventions.
The Suicide Rate Paradox
Contrary to expectations, SCZ patients with AS demonstrated a lower incidence of suicide attempts. This intriguing outcome raises questions about the protective factors that might be at play, including potential neurobiological differences. The brain's limbic system, which governs emotional regulation, may exhibit unique structural variations in patients with autism, impacting their suicide risk and necessitating further research.
Navigating the Insomnia-Suicide Link
Insomnia’s connection to suicide attempts is well-documented. Disturbing sleep patterns dramatically heighten risk, suggesting that understanding the mechanisms behind this relationship could offer critical insights for prevention strategies. As researchers probe deeper, topics like serotonin levels and its role in both sleep and mood regulation come to the forefront.
The Complicated Role of Autism Symptoms
Interestingly, the study suggests that AS might serve as a moderator in the insomnia-suicide attempt relationship, with insomnia scores correlating only in SCZ patients without AS. This points towards the intricate ways autism traits might alter risk profiles and highlights the need for future investigations to clarify these dynamics.
Moving Forward: Limitations and Future Needs
Despite its pioneering approach, this study has limitations, including its cross-sectional design and reliance on self-reported assessments. Future research must adopt more comprehensive methodologies to validate these findings and explore the deeper connections between insomnia, suicide risk, and autism symptoms in SCZ patients. As we strive to understand these complex interactions, targeted interventions will become increasingly essential in offering effective treatment to those in need.









 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)