Sepsis in Burn Patients: A Hidden Danger Exposed!
2025-09-01
Author: Sophie
The Global Burn Epidemic: An Underestimated Threat
Burn injuries affect a staggering 9 million individuals globally every year, constituting up to 20% of casualties in conflicts since World War II. Among military personnel, a shocking 18% of burn victims develop infections, with 69% suffering from multiple infections. Severe burns compromise the skin—the body’s frontline defense—dramatically increasing the chances of infection, especially for those with burns covering 20% or more of their total body surface area (TBSA), where infection rates can soar to a chilling 55%.
Sepsis: The Silent Killer in Burn Treatment
Sepsis, as defined by the Sepsis-3 guidelines, refers to a life-threatening organ dysfunction resulting from a chaotic response to infection. This can lead to dire consequences, including circulatory collapse and severe metabolic disturbances, often culminating in septic shock—a state that significantly heightens mortality risk. Despite advancements in treating burn injuries, sepsis remains the leading cause of death among these patients, with incidence rates for burns over 20% TBSA ranging from 3% to 39%.
A Call for Better Identification and Treatment
Sadly, the actual occurrence and outcomes of sepsis in burn patients are poorly documented, as many studies involve small sample sizes. Recent initiatives aim to sharpen the definitions and diagnostic criteria for sepsis, yet effective early identification remains elusive due to inadequate sensitivity and specificity in existing scoring systems.
The Vulnerable Population: Older Adults at Greater Risk
Older adults, in particular, face a heightened risk of severe complications, including sepsis, after burn injuries. Their compromised immune responses lead to increased mortality, multi-organ failure, and prolonged healing. Notably, data on diagnosing and treating sepsis in this demographic is scarce, suggesting an urgent need for focused research.
A Groundbreaking Study on Sepsis in Burn Patients
A recent retrospective study at the prestigious Ross Tilley Burn Centre and Hamilton Health Sciences Burn Unit has thrown open the curtains on sepsis prevalence in both adult and older adult burn patients. By scrutinizing a large cohort of 1,465 individuals, the research got to the heart of the critical factors influencing sepsis and its dire consequences.
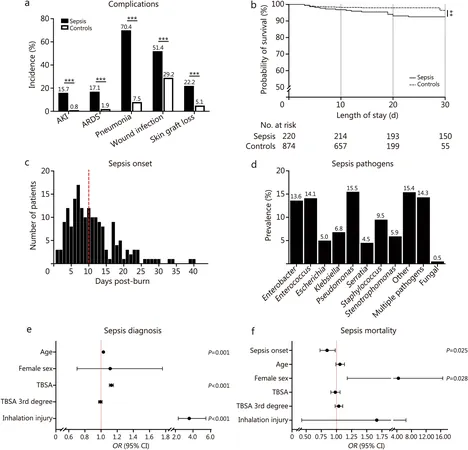
Sepsis Rates Shockingly High Among Burn Victims
The study revealed that 20.1% of adult burn patients were diagnosed with sepsis during hospitalization—this figure rose to 22.9% among older adults. The mortality rates were alarming: 7.3% for adults and 25.9% for older adults, indicating that prompt diagnosis and treatment can make a world of difference.
Compelling Insights: Predictors of Sepsis and Mortality
Age, burn size, and the presence of inhalation injury stood out as significant predictors of sepsis diagnoses across both age groups. Notably, a delay in sepsis onset drastically decreased mortality risk, highlighting the importance of early identification.
Understanding the Underlying Causes: A Step Towards Improvement
This groundbreaking study demonstrates the pressing need for immediate intervention strategies for those at high risk of sepsis, including closer monitoring for vulnerable groups. Optimizing potential early warning systems could enhance outcomes significantly, particularly for older patients.
Conclusion: A Call to Action for Burn Care Protocols
As we unravel the complexities surrounding sepsis in burn patients, this research is a timely reminder of the urgent need for improved detection and care protocols. It advocates for age-tailored sepsis management strategies, paving the way for better outcomes and reduced mortality rates in a patient population that cannot afford to wait.






 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)