New Research Links Inflammatory Burden Index to Rising Depression Rates: A Call to Action for Mental Health Awareness
2025-03-31
Author: William
Background
Depression has become a significant public health concern, intricately linked to systemic inflammatory responses in the body. Recent research has introduced the Inflammatory Burden Index (IBI) as a novel and comprehensive metric for assessing systemic inflammation. This groundbreaking study aims to evaluate the relationship between IBI and depression within the American population, shedding light on potential new avenues for diagnosis and treatment.
Methods
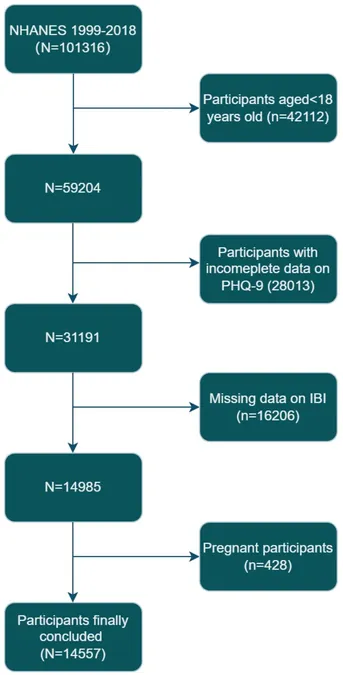
The study utilized data from the National Health and Nutrition Examination Survey (NHANES), encompassing years from 1999 to 2018. By calculating IBI through the formula (C-reactive protein × neutrophils/lymphocytes), researchers employed multivariate logistic regression to elucidate the correlation between IBI levels and depression prevalence. The analyses included subgroup evaluations, interaction tests, and sensitivity checks to ensure robust findings.
Results
Among the 14,557 participants analyzed, a notable 8.5% (1,231 individuals) were diagnosed with depression. The results revealed a striking linear correlation between elevated IBI and increased depression rates, with subjects in the highest tertile of IBI exhibiting a 40% higher incidence of depression compared to those in the lowest tertile. This correlation persisted across different demographic groups. Even after excluding extreme IBI values, the relationship remained consistent, suggesting a reliable association between inflammation and mental health.
The findings underscore the pressing need for identifying novel biomarkers to improve the prevention and intervention strategies for depression, which has witnessed a staggering 49.86% increase in global incidence from 1990 to 2017, as reported by the Global Burden of Disease data.
Conclusion
This study highlights a significant connection between IBI and depression among American adults, advocating for further large-scale prospective research. Depression is increasingly recognized as a multifaceted disorder, and understanding its correlation with systemic inflammation could pave the way for innovative treatment options.
Research indicates that inflammation may play a pathological role in the onset of depression, affecting the production of crucial neurotransmitters like serotonin and dopamine. Chronic stress is known to activate inflammatory processes, leading to alterations in mood and emotional regulation pathways, which can further exacerbate the severity of depressive disorders.
The traditional tools of measuring inflammatory markers, like C-reactive protein (CRP) and neutrophil-lymphocyte ratios, may not encapsulate the complexity of how inflammation interacts with mental health. Therefore, IBI, which integrates a broader spectrum of immune responses, could serve as a more effective diagnostic marker for mental health professionals.
Notably, women are disproportionately affected by depression, aligning with the study's findings that female participants had higher rates of depression compared to their male counterparts. The consequences of depression are profound, impacting not only individuals' mental health but also their physical well-being, leading to higher healthcare costs and decreased productivity.
As we delve deeper into the correlation between inflammation and depression, one can’t help but wonder: are we on the brink of a new era in mental health treatment? Future research will be critical in confirming these findings and possibly leading to breakthrough interventions aimed at modulating inflammation to alleviate depression symptoms. Experts agree that any advancement in understanding how inflammation contributes to mental health vulnerabilities could revolutionize treatment strategies, offering hope for millions worldwide struggling with depression.
In conclusion, the discovery of the link between the Inflammatory Burden Index and increased depression rates not only enhances our understanding of mental health but also invites a re-evaluation of our current approaches to treatment and prevention. As the prevalence of depression continues to rise, the time for action is now, compelling healthcare providers and policymakers to prioritize mental health initiatives informed by this pivotal research.








 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)