Mpox Cases in Congo Show Signs of Stabilization, WHO Reports - But Is the Threat Truly Over?
2024-11-11
Author: Olivia
Mpox Cases in Congo Show Signs of Stabilization, WHO Reports
In a startling update from the World Health Organization (WHO) on Monday, officials indicated that mpox cases in the Congo, particularly in South Kivu where a more transmissible variant was first detected, may be "plateauing." This positive trend, however, contrasts sharply with rising infection rates in other regions of the Congo, as well as in neighboring Burundi and Uganda.
The WHO report highlighted that while the overall number of mpox infections is on the rise, the situation in South Kivu—an area notorious for its gold mining activities—has stabilized. This region was initially a hotspot for the outbreak due to the interactions between sex workers and miners. Despite the plateauing figures in some areas, the broader narrative remains concerning as the virus continues its spread across the continent.
Current data indicates that Congo has reported fewer than 100 laboratory-confirmed mpox cases recently, a notable decrease from nearly 400 reported in July. Experts believe this decline offers a crucial opportunity for health authorities to intensify their efforts in controlling and potentially eradicating the outbreak.
Immunization efforts are underway, with around 50,000 individuals in Congo already vaccinated against mpox. However, the Africa Centers for Disease Control and Prevention (CDC) warns that an estimated 3 million vaccines are necessary to effectively halt the outbreak and prevent further escalation.
Dr. Jean Kaseya, director of the Africa CDC, emphasized that the continent is still grappling with the "acute phase" of the mpox epidemic, which currently impacts 19 countries. His cautionary note stressed that without significant resource allocation, the situation could evolve into a global concern.
The situation in Burundi is particularly alarming, with the new variant causing milder symptoms—thus allowing infectious individuals to unknowingly contribute to its spread. The country has reported over 200 new mpox cases weekly in recent weeks, predominantly affecting children and young adults.
In Uganda, the landscape is similarly perplexing, as recent reports confirmed over 100 new cases, primarily transmitted through sexual contact, indicating a demographic largely affected is adult populations.
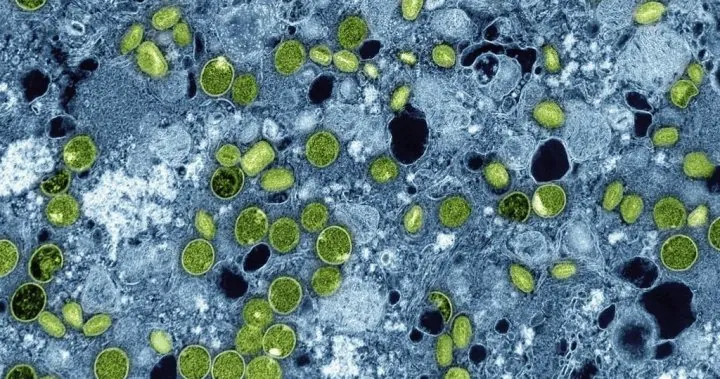
Mpox, previously known as monkeypox, initially drew its name from the animals used in early studies of the virus. Today, it spreads mainly through close skin-to-skin contact, with infected individuals potentially leaving traces on contaminated clothing or bedding. Often resulting in visible lesions, those infected may find themselves ostracized due to the apparent nature of the disease.
In August, WHO declared the rapid spread of mpox a global health emergency, underscoring the urgency of addressing the outbreak. To date, Africa has logged more than 46,000 suspected cases, alongside over 1,081 fatalities attributed to the virus.
The WHO is set to conduct an expert meeting on November 22 to assess whether mpox continues to represent an international emergency or if the danger has subsided. Meanwhile, vigilance remains paramount, as the virus has recently shown its capacity to spread beyond Africa; the UK reported its first case of the new variant from an individual recently returned from Africa, alongside infected contacts now receiving treatment in London hospitals.
As the fight against mpox continues, the pressing question remains: Are we truly turning the tide against this virus, or is a more formidable challenge looming on the horizon?





 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)