Is Microultrasonography the Future of Prostate Cancer Detection? Here’s What You Need to Know!
2025-03-24
Author: Liam
Recent groundbreaking research has unveiled that microultrasonography-guided biopsies may be just as effective as the standard magnetic resonance imaging (MRI)-guided biopsies for detecting clinically significant prostate cancer (csPCa) in biopsy-naïve men.
In a pivotal international multicenter, phase 3 randomized study published in the Journal of the American Medical Association (JAMA), researchers evaluated different biopsy techniques—microultrasonography, MRI combined with conventional ultrasound, and a hybrid of microultrasonography and MRI—across a cohort of 678 men, all new to prostate biopsies. The participants had a median age of 65 and exhibited a median prostate-specific antigen (PSA) level of 6.9 ng/mL.
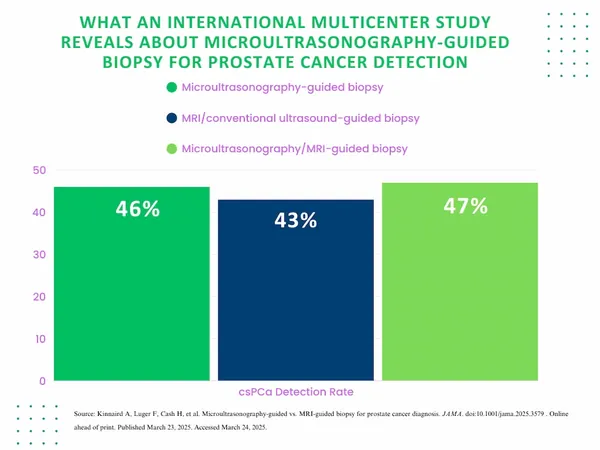
The results were eye-opening: microultrasonography-guided biopsies successfully identified csPCa in 46% of patients, while MRI/conventional ultrasound-guided biopsies detected it in 43% of cases. The combination technique saw the highest detection rate at 47%. Importantly, the differences among these methods were not statistically significant, indicating that microultrasonography could serve as a robust alternative.
Dr. Adam Kinnaird, the study's lead author from the University of Alberta, highlighted the clinical implications of these findings. “Microultrasonography offers a novel imaging and biopsy methodology that could significantly enhance accessibility for patients, particularly those unable to undergo an MRI,” he stated, emphasizing the benefits of a single-session procedure. This not only eliminates the need for contrast agents—often associated with complications—but also cuts down on wait times and costs, effectively reducing patient anxiety.
Microultrasonography boasts a remarkable imaging resolution of 70 microns (0.07 mm), which is a staggering 300% improvement over conventional ultrasound techniques. This high resolution enables clinicians to observe prostate cancer in real-time, improving accuracy and reducing errors linked to image registration. It allows for more detailed visualization of cancerous changes within prostate ducts.
However, the researchers did note a learning curve associated with the new technology. Physicians involved in the study underwent advanced training in microultrasonography to ensure proficiency. There is also an ongoing discussion regarding the Prostate Risk Identification using Micro-Ultrasound (PRI-MUS) scoring system, which, unlike the frequently revised PI-RADS scoring system for MRI, has yet to undergo extensive modifications.
Despite these promising results, the study did acknowledge limitations, such as the lack of blinding concerning the techniques used and the varying standards of MRI/ultrasonography fusion devices among participating centers. Additionally, the research mandated biopsies for all participants, contrasting with regular practices that often avoid biopsies in patients with low PI-RADS scores.
In summary, the evidence suggests that microultrasonography-guided biopsy could revolutionize prostate cancer detection, offering a swift and effective alternative to traditional MRI-guided methods. As the medical field continues to explore the potential of this innovative technique, patients and clinicians alike should stay informed about these developments that could change the landscape of cancer diagnostics. Keep your eyes peeled—this may be the breakthrough we've been waiting for!







 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)