Groundbreaking Discovery: Talaromyces Marneffei's Role in Central Nervous System Infections Among AIDS Patients!
2024-12-23
Author: Emily
Introduction
In a remarkable case emerging from Southern China, a 35-year-old woman battling AIDS was diagnosed with a rare and severe infection of the central nervous system (CNS) caused by the fungus Talaromyces marneffei. Exhibiting alarming symptoms over a span of 15 days, she was admitted with complaints of dizziness, headaches, fatigue, and respiratory issues, which raised concerns of multiple infectious diseases.
Diagnosis and Initial Findings
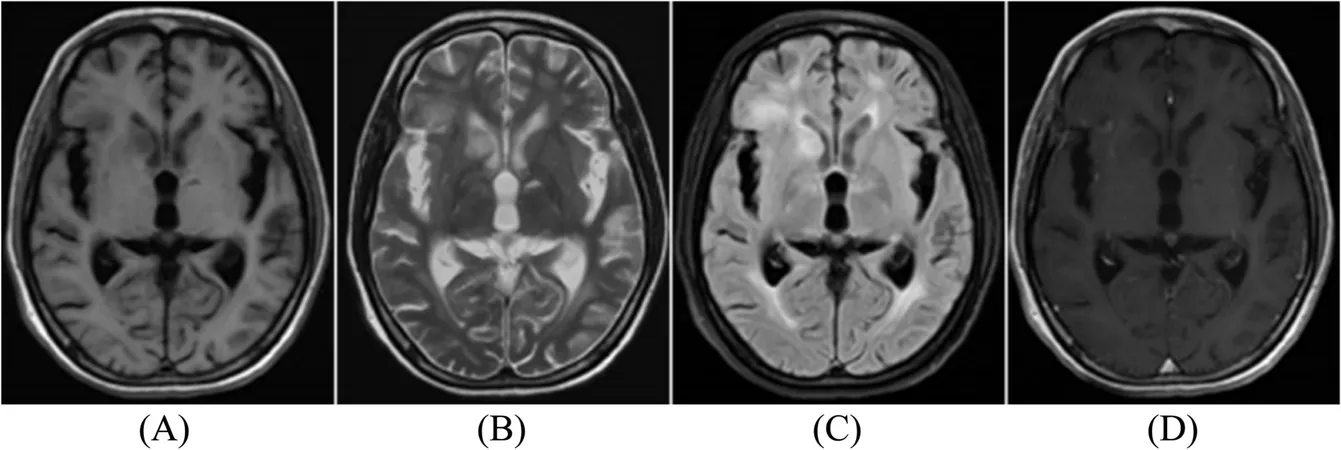
Upon hospital admission, physical examinations unveiled troubling signs: she had reduced consciousness, noticeable signs of meningeal irritation, and oral candidiasis. Diagnostic imaging via MRI revealed significant intracranial lesions and signs of cerebral atrophy, while her chest CT highlighted concerning changes in lung structure that suggested more complex infections.
Laboratory Investigations
Comprehensive laboratory testing pointed to an alarming immune status; her CD4 count was critically low at just 23 cells/mL, classifying her condition as advanced AIDS. Her erythrocyte sedimentation rate (ESR) skyrocketed, indicating systemic inflammation. Furthermore, HIV viral loads were dangerously high, prompting the medical team to consider possible tuberculosis and other bacterial infections.
Critical Lumbar Puncture
A pivotal lumbar puncture procedure was conducted, revealing clear cerebral spinal fluid (CSF) with elevated leukocyte levels and an alarming drop in glucose concentration. This anomaly, coupled with positive detection of the Mp1p antigen—specific to T. marneffei—blatantly confirmed the fungal infection.
Treatment Response and Complications
As her prognosis grew dire, she was treated rapidly with intravenous medications, including Mannitol to alleviate intracranial pressure and Amphotericin-B for antifungal therapy. Remarkably, her symptoms began to resolve after 7 days of treatment. However, complications arose when a re-evaluation seven weeks post-admittance finally confirmed the presence of Mycobacterium tuberculosis in her bronchoalveolar lavage fluid.
Implications for Future Diagnosis
This case underscores a critical gap in the diagnosis and treatment of CNS infections linked to endemic mycoses in AIDS patients. Typically overlooked due to their rarity, infections such as those caused by T. marneffei can mimic other conditions, complicating clinical recognition and timely intervention. Alarmingly, delays in diagnosis can increase mortality by up to 2% per day, highlighting an urgent need for improved detection methods.
Advancements in Diagnostic Techniques
New antigen detection tests, like the newly applied Mp1p assay—highly specific and sensitive for T. marneffei—could transform how doctors diagnose CNS infections in immunocompromised patients. Notably, the Mp1p antigen had not only been useful in diagnosing blood samples but was also successfully detected in this patient's CSF, paving the way for potential future diagnostic protocols.
Conclusion and Recommendations
The complexity of diagnosing CNS infections in the context of AIDS illuminates the need for heightened awareness and advanced diagnostic techniques. As only 32 cases of AIDS-related T. marneffei CNS infections have been documented globally, this case serves as a pivotal reminder of the challenges and advancements needed in infectious disease management among vulnerable populations.
Doctors are now urged to consider testing for Mp1p when patients present with neurological symptoms in endemic regions. Immediate brain imaging and CSF cultures should accompany this antigen test to provide comprehensive care. As the medical community continues to grapple with these multi-faceted fungal infections, this case marks a crucial step toward more effective interventions and better patient outcomes.
Stay updated as we continue to uncover insights in the battle against AIDS-induced infections, ensuring that no patient’s suffering goes unnoticed!






 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)