Empowering or Ensnaring? Insightful Findings from Caregivers and Dementia Patients on Intelligent Assistive Technologies
2025-04-05
Author: Emma
Introduction
Intelligent Assistive Technology (IAT) is emerging as a game-changer in dementia care, offering tools like GPS devices, smart home systems, and memory aids designed to boost autonomy and improve the quality of life for individuals with dementia. These technologies are seen as a way to support independent mobility, enhance safety, and alleviate caregiver stress. Studies have revealed that tools for emergency assistance, navigation, and communication can significantly benefit both caregivers and dementia patients by fostering an environment that reduces anxiety and enhances independence.
Ethical and Social Challenges
However, while many perceive IAT as beneficial, there are important ethical and social challenges to consider. Critics express concerns over the potential for these technologies to infringe on patient privacy, create new dependencies, and inadvertently foster patronization. The very essence of empowerment — the ability of individuals with dementia to exercise their own decisions — is called into question as some technologies may unintentionally limit personal freedoms.
The Concept of Empowerment in Dementia Care
As caretakers and healthcare practitioners increasingly embrace a person-centered and empowering approach to dementia care, the concept of "empowerment" has gained traction. It is about not just technology's potential to improve life quality but also ensuring that it aligns with the actual needs and desires of individuals. Empowerment provides a framework that incorporates individual vulnerabilities and dependencies, highlighting the balance of power in the caregiver-care recipient relationship.
Study Overview
Our latest study explores the perspectives of dementia patients and their caregivers in Germany regarding three specific IATs: a GPS bracelet for outdoor mobility, emotion recognition technology designed to detect and address negative feelings, and an intelligent dressing device. Each device addresses different aspects of daily living — from practical functions to emotional well-being — offering a comprehensive view of their implications.
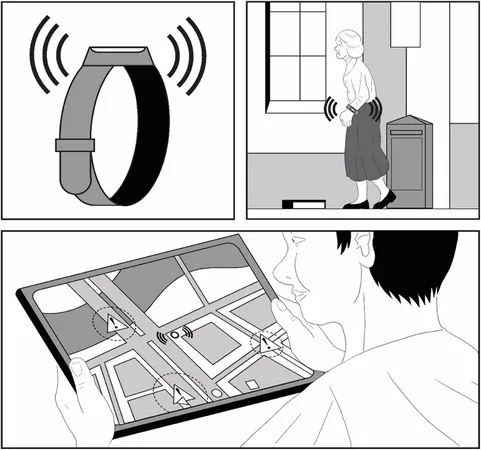
Findings on GPS Bracelet
Through semi-structured interviews with 27 individuals — 12 persons with dementia and 15 family caregivers — we found that the GPS bracelet is appreciated for its potential to promote independence. Interviewees felt it could enhance safety and mobility, granting patients the freedom to move without constant human supervision. Yet, concerns were raised about the potential risks of surveillance, with many expressing that they would rather retain their privacy, even at the cost of some independence.
Concerns with Emotion Recognition Technology
With emotion recognition technology, participants voiced similar apprehensions about privacy violations due to constant monitoring of their emotional states. While some caregivers saw the benefit in reducing conflicts and improving relationships, there was widespread fear that technological oversight could reduce genuine human empathy and interaction. Caregivers expressed discomfort regarding the ethical implications of monitoring, especially without explicit consent from the patients.
Skepticism Towards Intelligent Dressing Technology
The intelligent dressing technology aimed to provide support in independently dressing, yet skepticism loomed large. Many felt that the technology might not be practical or user-friendly and could undermine social interactions, a crucial aspect of care for people with dementia. Both dementia patients and caregivers emphasized the importance of human interaction over technological solutions, fearing that IAT could lead to increased isolation instead of fostering social engagement.
Conclusion and Future Directions
Our findings indicate a nuanced view among dementia patients and caregivers regarding IAT. While there is optimism about its potential to enhance independence, significant reservations persist regarding privacy, autonomy, and the overall emotional landscape of care. With the goal of integrating these insights into future technology designs, it’s evident that participatory research—actively involving both caregivers and patients in the co-design of assistive technologies—is crucial for creating effective, user-centered solutions.
Ultimately, this study reveals that while Intelligent Assistive Technologies hold significant promise for supporting individuals with dementia, their actual implementation requires careful consideration of ethical implications, individual user needs, and a holistic view of care dynamics. The potential benefits, if realized alongside a commitment to empowerment, could lead to transformative improvements in the lives of those with dementia and their caregivers.







 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)