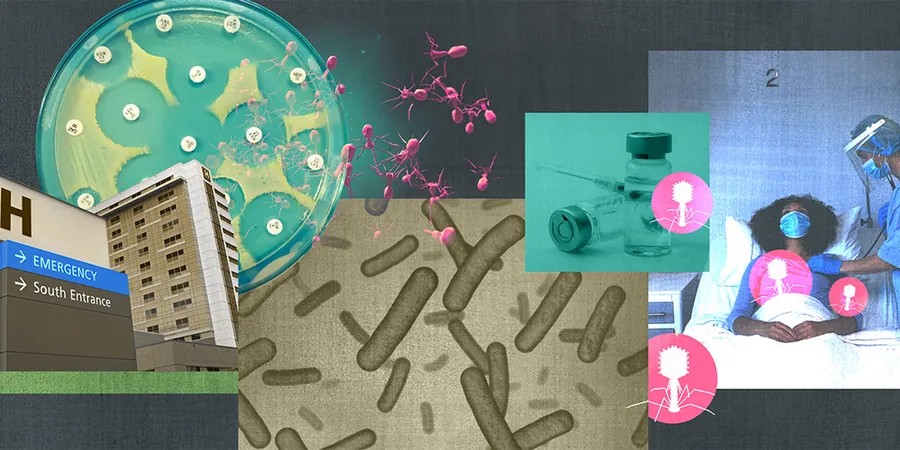
Are We on the Brink of Defeating Antibiotic Resistance with Bacteriophages?
2025-01-19
Author: Charlotte
Are We on the Brink of Defeating Antibiotic Resistance with Bacteriophages?
In a pioneering moment of microbiological discovery back in 1910, Franco-Canadian scientist Félix d'Hérelle observed something extraordinary under his microscope: "clear spots" that were revealed to be bacteriophages—viruses that target and destroy bacteria. This groundbreaking revelation led to the use of these phages as a treatment method for bacterial infections, including dysentery, during the aftermath of World War I. While this innovative therapy was effective for illnesses like bubonic plague, it eventually faded into obscurity as antibiotics gained popularity in the 1940s.
Fast forward to today, and the world faces a formidable challenge: rising antibiotic resistance among bacteria, which has made treating even common infections exceedingly difficult. An alarming statistic shows that more than 70% of hospital-acquired bacterial infections in the United States are now resistant to at least one antibiotic. With antibiotic-resistant bacteria such as Acinetobacter and Klebsiella formally categorized as critical threats by the World Health Organization, the urgency for alternative solutions has never been greater.
In recent developments, researchers are revisiting phage therapy but with an innovative twist: "phage steering." This modern approach seeks to engender an evolutionary conundrum for bacteria, forcing them to confront both phages and antibiotics simultaneously—an act that could lead to their demise.
Initial studies utilizing phage steering have yielded promising outcomes. Notably, a 2023 study led by Paul Turner at Yale University demonstrated that exposing multidrug-resistant Pseudomonas aeruginosa to a specific phage, OMKO1, rendered these bacteria more vulnerable to antibiotics than those that had never encountered the phage. The mechanism behind this success lies within the bacterial efflux pumps—structures that bacteria modify to expel antibiotics. Turner’s hypothesis suggests that if the bacteria attempt to adapt to evade the phage's attack, they potentially lose their ability to eliminate the antibiotics, placing themselves in a precarious position.
Excitingly, Turner’s research revealed that his team’s application of phage steering in patients displayed significant efficacy in reducing antimicrobial resistance. Even as some of the results remain unpublished, anecdotal evidence indicates marked improvement in clinical cases, especially in non-respiratory infections.
However, researchers are cognizant of the complexities associated with phage therapy. Despite the encouraging findings, molecular biologist Graham Hatfull notes that success is not guaranteed for all bacterial strains—much depends on the specificity and binding efficiency of the phages to particular bacteria. In fact, phages are notorious for being host-specific; identifying the right phage for each infection is challenging, often requiring rigorous testing.
Astonishing successes have been documented, such as one case where a patient with a lethal A. baumannii infection regained consciousness merely days after phage therapy was initiated, subsequently responding to previously ineffective antibiotics. Yet, simultaneous experiments in vitro did not replicate this success, indicating that the relationship between phage resistance and antibiotic sensitivity can be unpredictable.
The evolution of phage therapy may still face hurdles, such as the risk of triggering severe inflammatory responses in patients if phages kill bacteria too rapidly or if they mutate in ways that undermine treatment efficacy. Due to these potential dangers and the lack of precision compared to conventional antibiotics, phage therapy remains largely experimental in countries like the U.S.
Despite the challenges, the revival of bacteriophage use offers hope in our ongoing battle against antibiotic resistance. As researchers work towards refining and understanding this therapy, we stand at the cusp of a healthcare revolution that could reshape our approach to infectious diseases. The quest for effective solutions continues, and the re-emerging world of phage therapy may just hold the key to turning the tide against one of modern medicine's most pressing crises.







 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)