Alarming Surge: Ontario Faces Multi-Drug Overdose Crisis Amidst Shift in Treatment Approach
2025-01-09
Author: Jacques
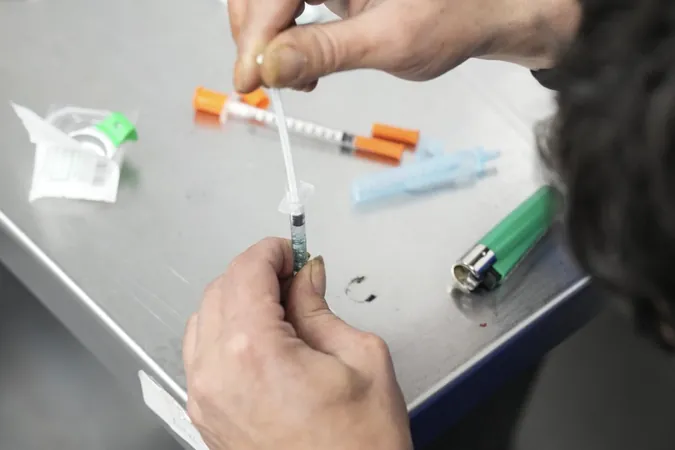
TORONTO — A troubling new report highlights the growing trend of overdose deaths in Ontario involving multiple drugs, particularly the dangerous combination of opioids and stimulants. The study, conducted by the Ontario Drug Policy Research Network and Public Health Ontario, reveals that the landscape of drug-related fatalities has evolved significantly since the onset of the COVID-19 pandemic.
Between 2018 and 2022, the monthly rate of overdose deaths attributed to a single drug surged by 75%. In stark contrast, fatalities involving two substances skyrocketed by 167%, and those associated with three or more drugs increased by an alarming 186%. The data indicates that over 12,115 accidental overdose deaths occurred in Ontario during this period, primarily stemming from opioids, stimulants, alcohol, and benzodiazepines.
Tara Gomes, an epidemiologist with Unity Health and a key author of the report, emphasized the emerging patterns, stating, “The most common situation is that opioids and stimulants together are contributing to death.” Yet, the rise in cases where opioids, stimulants, and benzodiazepines or alcohol interact is particularly worrisome as it complicates the response to overdoses.
Opioids, mainly illicit fentanyl, were involved in nearly 84% of drug toxicity deaths, accounting for over 10,000 victims. Stimulants contributed to around 62% of overdose fatalities, while alcohol and benzodiazepines accounted for 13% and 9%, respectively.
Researchers also investigated the health-care interactions of those who succumbed to overdoses. Notably, about one-third had some form of contact with the health-care system in the week leading up to their death, while 56% had engaged with health-care services within the previous month. This included visits to emergency departments and other medical facilities, highlighting a critical area for intervention.
Gomes expressed her concerns about the readiness of emergency departments to support individuals with addiction issues. “Most hospitals don't have addiction medicine specialists on site,” she noted, advocating for the expansion of addiction medicine consult services throughout the province. These programs aim to ensure that those struggling with substance use receive adequate care in emergency settings and facilitating proper post-discharge support.
The grim escalation of overdose deaths started around 2015 with the infiltration of illicit fentanyl into the drug supply. This situation intensified during the pandemic due to social isolation and disrupted access to health-care services. The blending of fentanyl with other substances, including benzodiazepines, has further complicated the crisis, with benzodiazepines increasingly linked to opioid-related fatalities.
The latest figures reveal a staggering number of more than 2,600 Ontarians lost their lives to opioids in 2023, according to Ontario's Office of the Chief Coroner.
In response to this burgeoning crisis, Ontario is set to change its strategy regarding opioid addiction and overdose prevention. The province will close 10 supervised consumption sites near schools and daycares by the end of March and plans to transition to an abstinence-based treatment model. New initiatives will include “homelessness and addiction recovery treatment hubs” by April 1, as well as the introduction of 375 supportive housing units at a cost of $378 million.
As Ontario grapples with this unprecedented multi-drug overdose crisis, experts call for urgent action and a reevaluation of current health policies to address the complex interplay of substances contributing to these tragic outcomes. Failure to adapt could mean even more lives lost in the fight against addiction.







 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)